Endovascular versus Medical Management of Acute Basilar Artery Occlusion: A Systematic Review and Meta-Analysis of the Randomized Controlled Trials
Article information
Abstract
Background and Purpose
The optimal management of patients with acute basilar artery occlusion (BAO) is uncertain. We aimed to evaluate the safety and efficacy of endovascular thrombectomy (EVT) compared to medical management (MM) for acute BAO through a meta-analysis of randomized controlled trials (RCTs).
Methods
We performed a systematic review and meta-analysis of RCTs of patients with acute BAO. We analyzed the pooled effect of EVT compared to MM on the primary outcome (modified Rankin Scale [mRS] of 0–3 at 3 months), secondary outcome (mRS 0–2 at 3 months), symptomatic intracranial hemorrhage (sICH), and 3-month mortality rates. For each study, effect sizes were computed as odds ratios (ORs) with random effects and Mantel-Haenszel weighting.
Results
Four RCTs met inclusion criteria including 988 patients. There were higher odds of mRS of 0-3 at 90 days in the EVT versus MM group (45.1% vs. 29.1%, OR 1.99, 95% confidence interval [CI] 1.04–3.80; P=0.04). Patients receiving EVT had a higher sICH compared to MM (5.4% vs. 0.8%, OR 7.89, 95% CI 4.10–15.19; P<0.01). Mortality was lower in the EVT group (35.5% vs. 45.1%, OR 0.64, 95% CI 0.42–0.99; P=0.05). In an analysis of two trials with BAO patients and National Institutes of Health Stroke Scale (NIHSS) <10, there was no difference in 90-day outcomes between EVT versus MM.
Conclusion
In this systematic review and meta-analysis, EVT was associated with favorable outcome and decreased mortality in patients with BAO up to 24 hours from stroke symptoms compared to MM. The treatment effect in BAO patients with NIHSS <10 was less certain. Further studies are of interest to evaluate the efficacy of EVT in basilar occlusion patients with milder symptoms.
Introduction
Endovascular thrombectomy (EVT) has become the standard of care for acute ischemic stroke due to large vessel occlusion (LVO) in the anterior circulation up to 24 hours from symptom onset after the publication of several randomized trials between 2015 and 2018 [1-7]. Patients with posterior circulation stroke were underrepresented in these trials [8,9]. The efficacy and safety of EVT in posterior circulation stroke has been debated [10,11]. Posterior circulation strokes, particularly those due to acute basilar artery occlusion (BAO), are devastating with high morbidity and mortality rates reaching up to 83%–96% in the absence of reperfusion [12,13]. EVT was reported with good clinical outcomes in acute BAO with rates of favorable functional outcome (modified Rankin Scale [mRS] score 0–3) at 90 days ranging between 32% to 40% in two prospective studies [14,15]. However, these studies were limited by selection bias, unblinded 90-day assessments, and heterogeneous treatment approaches [14-16]. Over the last three years, four randomized controlled studies (RCTs) reached different conclusions regarding the efficacy of EVT in acute BAO stroke [17-20]. In 2020 and 2021, the BEST (Basilar Artery Occlusion Endovascular Intervention versus Standard Medical Treatment) and BASICS (Basilar Artery International Cooperation Study) trials demonstrated that in patients with BAO, there was equivocal benefit of EVT as compared to medical management (MM) [17,18]. However, these trials were underpowered and had limitations that may have hindered the validity of their results. Recently, two RCTs (ATTENTION [Endovascular Treatment For Acute Basilar Artery Occlusion: A Multicentre Randomised Clinical Trial] and BAOCHE [Basilar Artery Occlusion Chinese Endovascular Trial]) showed benefit of EVT compared to MM for acute BAO up to 24 hours from stroke onset [19,20]. As these trials were of moderate size, pooling of their data may improve precision in the estimated treatment effect and reflect the diversity of patients across multiple countries. In this systematic review and study-level meta-analysis of these four RCTs, we aimed to analyze the clinical and safety outcomes in acute BAO patients treated with EVT compared to MM.
Methods
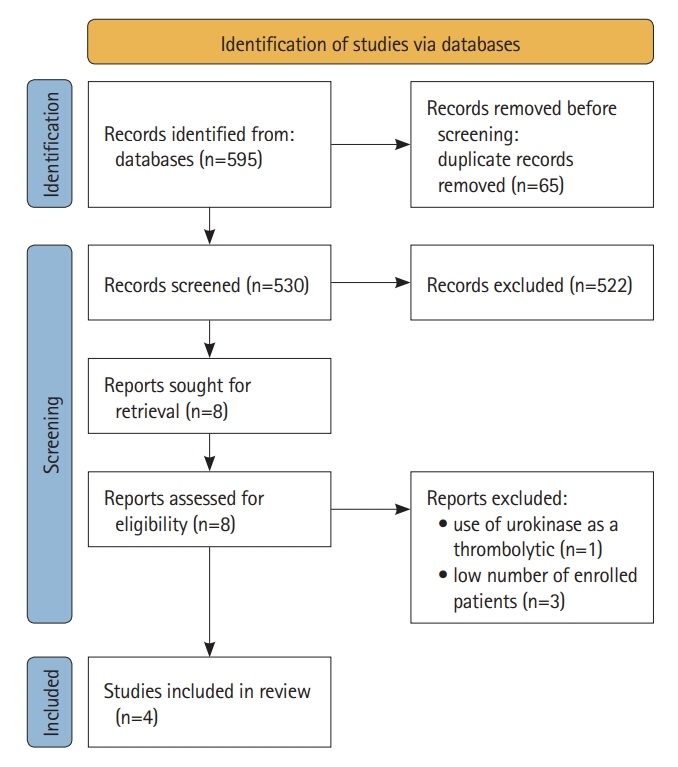
This systematic review and meta-analysis is presented according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [21]. The study protocol was registered on the International Prospective Register of Systemic Reviews on July 18, 2022 (PROSPERO CRD42022344565). Data are available on reasonable request to the corresponding authors.
Search strategy
The search was conducted with MEDLINE, EMBASE, Cochrane, and Web of Science using the following terms: (“Vertebrobasilar” OR “Vertebral” OR “Basilar”) AND (“Stroke” OR “Ischemia”) AND (“Thrombectomy” OR “Thrombolysis”) AND (“RCT” OR “randomized controlled trial”). In addition, the RCTs of LVO patients including the anterior circulation were searched for inclusion of patients with BAO. Abstracts and articles were identified and reviewed by two authors independently (MA and TNN). Disagreement was then discussed with a third author (SF).
Eligibility criteria
We included studies that reported EVT versus MM of patients with acute BAO stroke from January 1, 2000 to October 28, 2022. The inclusion criteria were as follows: (1) RCT, (2) interventional arm receiving EVT and MM, (3) control arm receiving MM, and (4) report of mRS score of 0–3 at 3 months, 90-day mortality, and symptomatic intracranial hemorrhage (sICH). Patients were treated with intravenous thrombolysis (IVT) if eligible before randomization. We excluded RCTs in which less than 50 patients with BAO were enrolled.
Data extraction
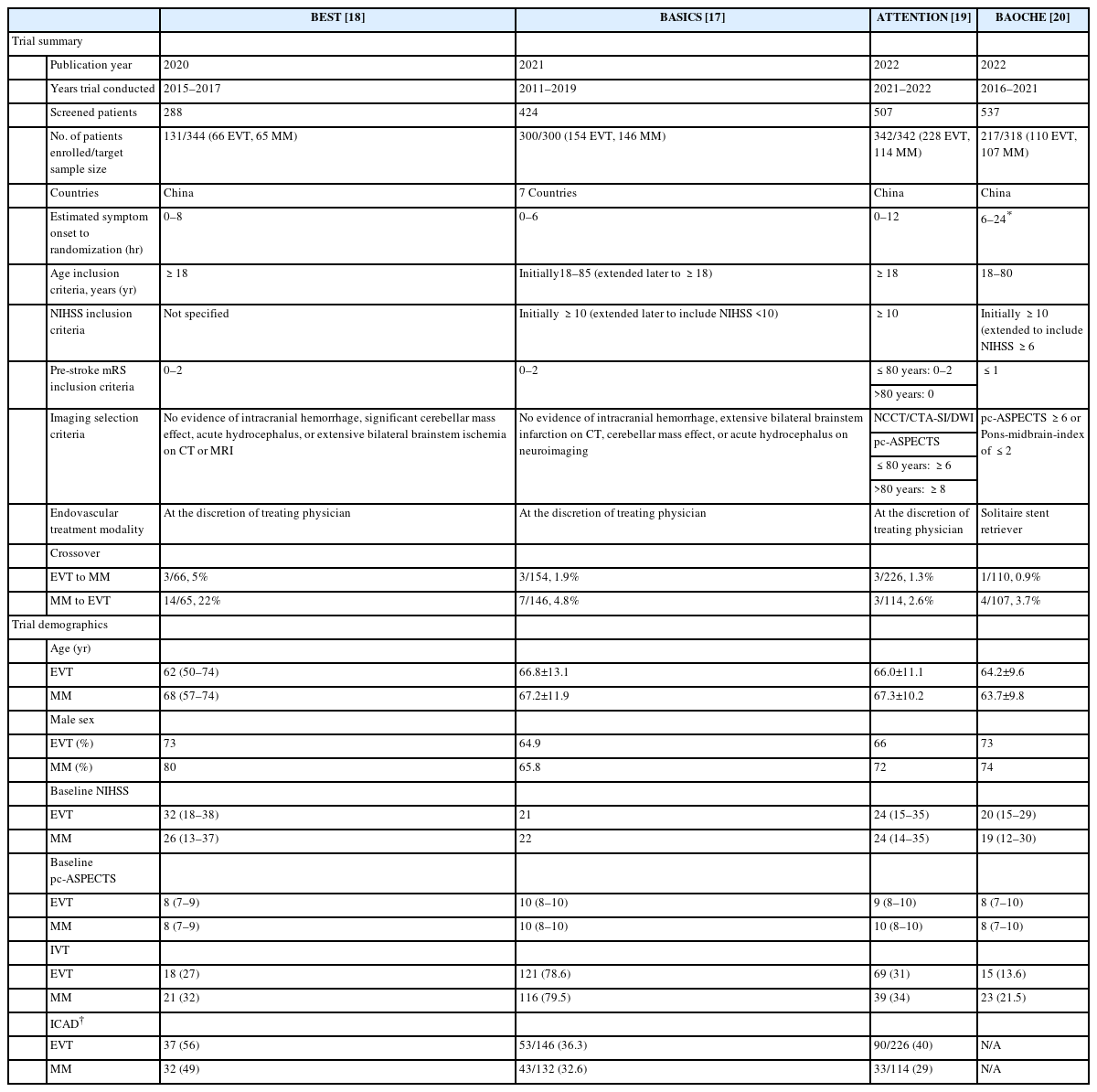
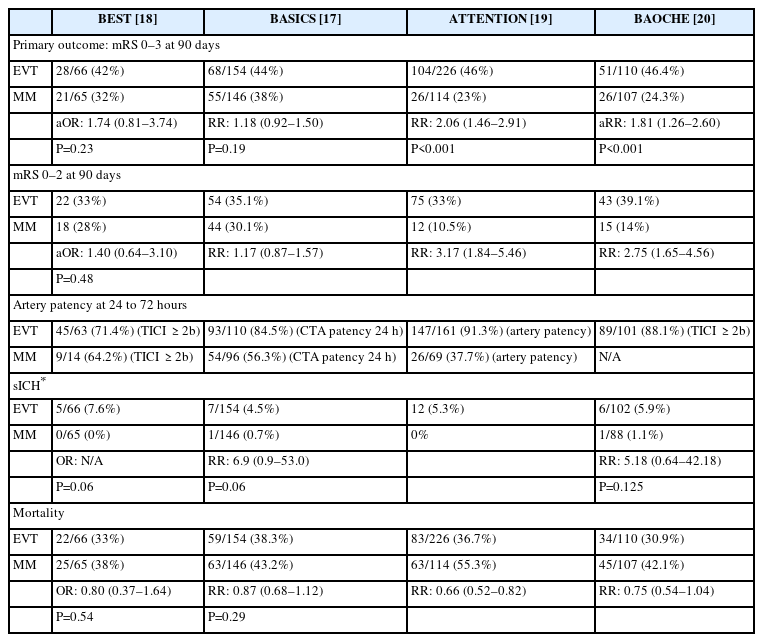
We collected patient characteristics including: age, sex, baseline National Institutes of Health Stroke Scale (NIHSS), IVT, baseline posterior circulation Alberta Stroke Program Early Computed Tomography Score (pc-ASPECTS), cross-over rate, endovascular technique, and recanalization rate (Table 1). Using data from the trials, we compared outcomes between the EVT and MM groups for four RCTs. Our pre-specified primary outcome was the proportion of patients with a favorable functional outcome defined as mRS of 0 to 3 at 90 days. Secondary outcomes included the proportion of patients who achieved excellent outcome (mRS of 0–2 at 90 days) after treatment. Safety outcomes included sICH as defined by each trial and 90-day mortality rate (Table 2). Supplementary data of the primary, secondary, and safety outcomes were obtained and analyzed from the BASICS and BAOCHE trials for patients with NIHSS <10.
Statistical analysis
Data were reported as intention-to-treat analysis. For each study, effect sizes were computed as logit transformed odds ratios (ORs) with random effects and Mantel-Haenszel weighting. The between-study variance component of random-effect models was estimated using restricted effects maximum likelihood with 95% confidence intervals (CIs). Because of the small number of patients included in the meta-analysis, 95% CIs around pooled effect sizes were calculated using Hartung-Knapp adjustment to provide a more conservative estimate of the true intervention and reduce the risk of false positives [22]. For each pooled result, Higgin I2 statistics were used to measure the percentage to the total variability in effect estimates attributed to heterogeneity rather than sampling error. The absolute value of the true variance in effect sizes is indicated by τ2 values in forest plots, estimated using restricted effects maximum likelihood. A funnel plot was used to evaluate potential publication or selection bias.
Results
Summary of included studies
The initial search strategy yielded eight RCTs (Figure 1). One RCT was excluded because of use of an older intra-arterial treatment (urokinase), which was terminated in 2005 after enrollment of 16 patients [23]. Three RCTs that included patients with both anterior and posterior circulation strokes were excluded because of the low number of BAO patients enrolled (10 patients in EASI [Endovascular Acute Stroke Intervention], 4 patients in THRACE [Mechanical Thrombectomy After Intravenous Alteplase versus Alteplase Alone After Stroke], and 4 patients in IMS III [Interventional Management of Stroke III]) [8,9,24]. After exclusion of these four trials, this yielded four published BAO RCTs meeting inclusion criteria with a total of 988 patients. A description of each trial’s inclusion, exclusion, and selection criteria is presented (Table 1).
Primary outcome
Across the four RCTs encompassing 988 patients, the primary endpoint of a favorable functional outcome (mRS of 0–3) at 90 days was achieved in 251 of 556 patients (45.1%, 95% CI 41%–49.3%) in the EVT group compared to 128 of 432 patients (29.6%, 95% CI 21.7%–36.4%) for the MM group (Figure 2A). The odds of a favorable functional outcome of mRS 0–3 were higher in the EVT compared to the MM group (OR 1.99; 95% CI 1.04–3.80, P=0.04). The between-study variability in effects estimates unrelated to sampling error was moderate (I2=54.65%, P=0.08).
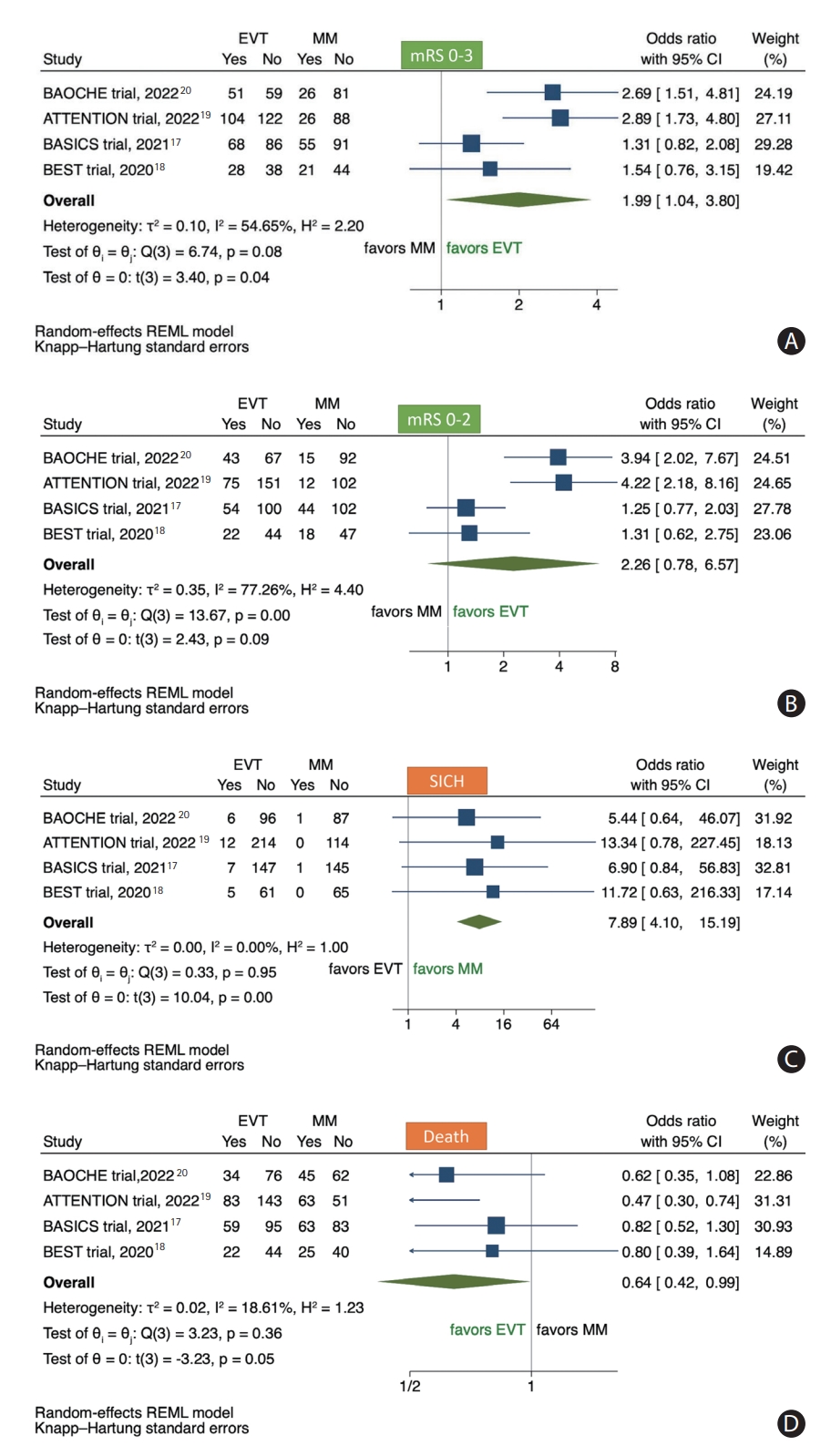
Forest plots for (A) favorable functional outcome (mRS 0–3) at 3 months, (B) excellent clinical outcome (mRS 0–2) at 3 months, (C) symptomatic intracranial hemorrhage, and (D) mortality odds ratio for pooled patient groups treated with EVT or MM. mRS, modified Rankin Scale; EVT, endovascular thrombectomy; MM, medical management; CI, confidence interval; BAOCHE, Basilar Artery Occlusion Chinese Endovascular Trial; ATTENTION, Endovascular Treatment For Acute Basilar Artery Occlusion: A Multicentre Randomised Clinical Trial; BASICS, Basilar Artery International Cooperation Study; BEST, Basilar Artery Occlusion Endovascular Intervention versus Standard Medical Treatment; REML, random effect restricted maximum likelihood.
Secondary outcome
Excellent clinical outcome (mRS of 0–2) occurred in 194 of 556 patients (34.8%, 95% CI 30.9%–38.8%) for the EVT group, and 89 of 432 patients (20.6%, 95% CI 10.4%–29.9%) for the MM group (Figure 2B). No statistical difference was observed in the odds of mRS 0–2 in the EVT compared to the MM group (OR 2.26; 95% CI 0.78–6.57, P=0.09). The between-study variability in effect estimates unrelated to sampling error was significantly high (I2=77.26%, P<0.01).
Safety outcome
The analysis of the pooled data showed an overall sICH rate of 5.4% (95% CI 3.5%–7.2%) for the EVT group, and of 0.8% (95% CI 0.0%–2%) for the MM group (Figure 2C). The EVT group had higher odds of sICH than the MM group (OR 7.89; 95% CI 4.10–15.19, P<0.01). The estimated between-study variability in effect estimates unrelated to sampling error was low (I2=0%, P=0.95).
The mortality rate in the EVT group was 198 of 556 patients (35.6%, 95% CI 31.5%–39.5%), and for the MM group 196 of 432 patients (45.4%, 95% CI 38.1%–52.1%) (Figure 2D). The EVT group had lower odds of mortality compared to the MM group (OR 0.64; 95% CI 0.42–0.99, P=0.05). The estimated between-study variability in effect estimates unrelated to sampling error was low (I2=18.61%, P=0.36).
Risk of bias
No evidence suggestive of publication bias was found by examining the funnel plots.
NIHSS <10 subgroup
Supplementary analysis of 78 patients with BAO and NIHSS <10 was obtained from the BASICS (n=61) and BAOCHE (n=17) trials. In this subgroup analysis, frequencies of favorable (mRS 0–3) or excellent (mRS 0–2) clinical outcome between the EVT and the MM groups were comparable. Favorable functional outcome (mRS of 0–3) at 90 days was achieved in 26 of 37 patients (70.3%) in the EVT group and in 30 of 41 patients (73.2%) for the MM group. Excellent clinical outcome (mRS of 0–2) occurred in 22 of 37 patients (59.5%) for the EVT group, and 24 of 41 patients (58.5%) for the MM group (Figure 3). The rate of sICH in patients with NIHSS <10 was 8.1% for the EVT group. There was no sICH for the MM group. The mortality rate in the EVT group was 18.9% (7 of 37 patients) which was comparable to that of the MM group (17.1%, 7 of 41 patients).
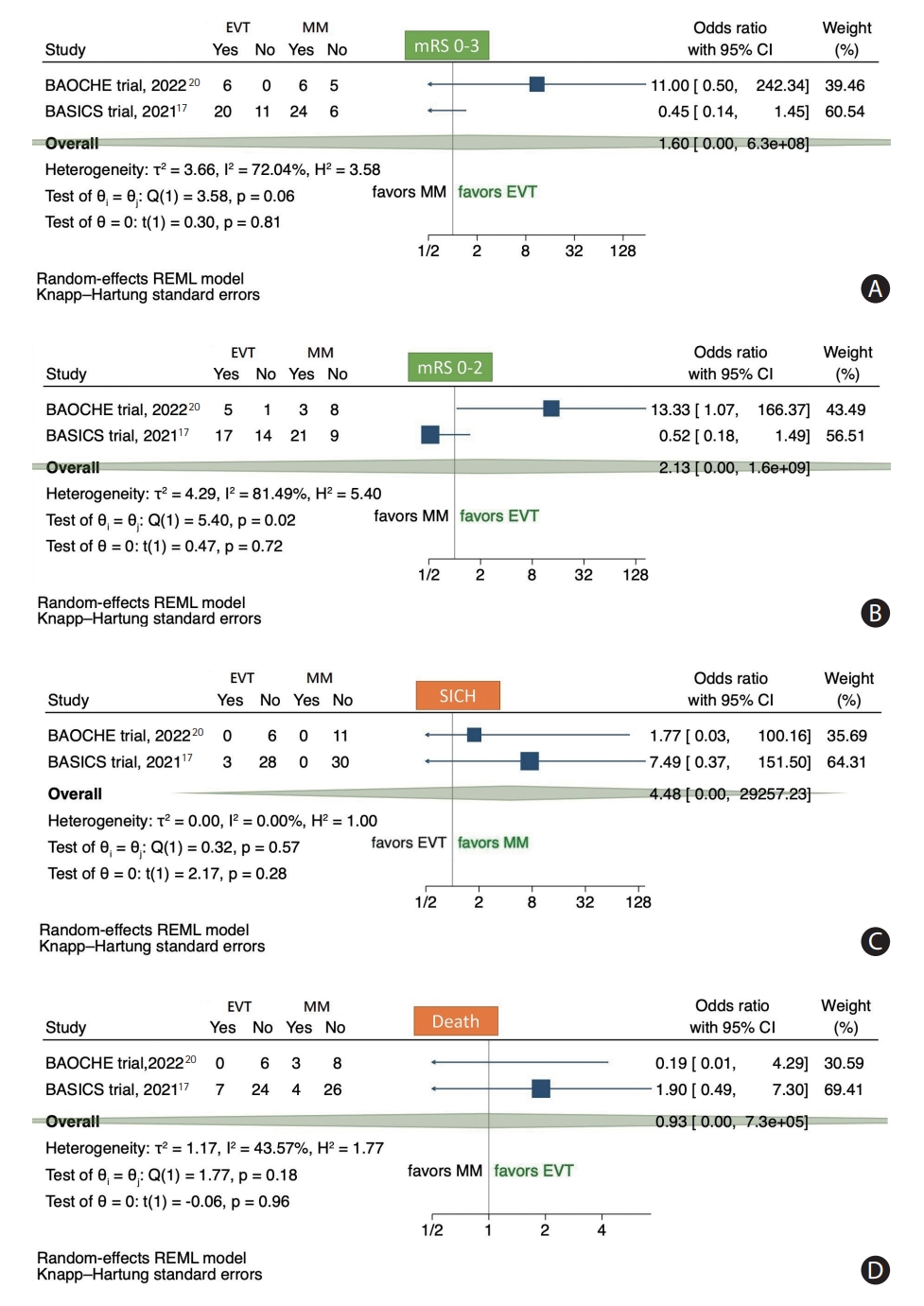
Forest plots for the (A) primary outcome data (mRS 0–3), (B) secondary endpoints of excellent clinical outcome (mRS 0–2), (C) symptomatic intracranial hemorrhage, and (D) mortality for patients with acute basilar occlusion and NIHSS <10 treated with EVT or MM. mRS, modified Rankin Scale; EVT, endovascular thrombectomy; MM, medical management; CI, confidence interval; BAOCHE, Basilar Artery Occlusion Chinese Endovascular Trial; BASICS, Basilar Artery International Cooperation Study; REML, random effect restricted maximum likelihood.
Discussion
In this intention-to-treat meta-analysis of the BEST, BASICS, ATTENTION, and BAOCHE randomized trials, we confirm that in patients with acute BAO stroke, there was a twofold increase in the odds of favorable outcome (mRS 0–3) at 3 months with EVT compared to MM. No difference was observed in the odds of excellent outcome (mRS of 0–2) in the EVT compared to the MM group, although the direction and magnitude of effect similarly favored EVT. An mRS 0–3 (rather than mRS 0–2) was likely chosen as the primary endpoint across the four BAO RCTs because it may be a more sensitive measure that accounts for the higher severity of BAO disease when patients are recovered. Despite an increase in sICH in the EVT group, patients treated with EVT had lower odds of mortality compared to the MM group. In subgroup analysis of 78 BAO patients with NIHSS <10, the frequency of favorable or excellent outcomes at 90 days as well as mortality was similar in the EVT as compared to the MM group while the frequency of sICH was 8.1% in EVT group compared to none in the MM group.
The overall results of this meta-analysis are in alignment with the two recent BAO RCTs (ATTENTION and BAOCHE) [19,20], which contrast with the initial neutral BAO RCTs (BEST and BASICS) [12,18]. BEST and BASICS encountered formidable challenges with enrollment, selection bias, and crossovers. Additionally, the original BASICS inclusion criterion of NIHSS ≥10 was modified during the trial to include patients with milder stroke deficits [25]. As was observed with the prospective BASICS and Helsinki registry studies [12,26], the BASICS RCT, with a high proportion of patients receiving IVT, revealed how well patients with mild stroke deficits can do with MM of BAO, thereby attenuating the potential treatment effect of EVT in the subgroup of BAO patients with low NIHSS. In the BEST trial, the progressive drop in recruitment over time, and the crossovers led to the premature termination of the trial by the data and safety monitoring board [18], hence reducing statistical power and lowering the treatment effect size for the intention-to-treat analysis. Moreover, the overwhelmingly positive anterior circulation trials favoring EVT published in 2015 may have led to a loss of equipoise in randomizing consecutive BAO patients into the trials, and thereby contributing to potential selection bias and the neutral BEST and BASICS trial results [17,18].
Perhaps as a result of the neutral trial results, BEST and BASICS provided the foundations to reinforce the concept of equipoise regarding EVT versus MM management of BAO patients [10,11]. BAOCHE and ATTENTION reinforced consecutive enrolment following the neutral results of BEST and BASICS, resulting in a high inclusion of eligible patients with BAO. In ATTENTION, 342 out of 507 screened patients were enrolled in 1 year compared to 300 patients in 8 years in BASICS. EVT in ATTENTION was discouraged outside of the trial. Extending the time windows up to 12 hours from estimated onset in ATTENTION and up to 24 hours in BAOCHE expanded the number of eligible patients for enrollment. The crossover rates were low in ATTENTION compared to the BEST trial (1.3% [3/226] crossed-over from EVT to MM in ATTENTION vs. 5% [3/66] in BEST; 2.6% crossed over from MM to EVT in ATTENTION compared to 22% in BEST). To decrease the risk of futile recanalization, both BAOCHE and ATTENTION trials used an imaging scale (pc-ASPECTS) [27] and included patients with small infarct at baseline (pc-ASPECTS ≥8 in ATTENTION and ≥6 in BAOCHE).
In ATTENTION, a twofold favorable outcome was achieved in the EVT compared to MM group, with a number needed to treat of 4 [19]. The disability reduction benefit of EVT in BAO patients in ATTENTION was comparable to the anterior circulation trials (90-day mRS ordinal shift analysis: OR 2.8 [95% CI: 1.8–4.4] in ATTENTION vs. 2.49 [1.76–3.53] in HERMES [Highly Effective Reperfusion Evaluated in Multiple Endovascular Stroke Trials] [28] and 2.54 [1.83-3.54] in AURORA [Analysis of Pooled Data from Randomized Studies of Thrombectomy More Than 6 Hours after Last Known Well] [29]). ATTENTION also demonstrated a potential mortality benefit to EVT treatment, in contrast to most anterior circulation EVT trials [19].
BAOCHE assessed the safety and efficacy of EVT versus MM for acute BAO in patients presenting in a 6 to 24 hour time window after symptom onset [20]. In BAOCHE, the proportion of patients achieving favorable outcomes defined as mRS 0–3 at 90 days was higher in the EVT versus MM group with a number needed to treat of 4.5. BAOCHE showed the benefit of BAO EVT in the extended window without increased risk of sICH [20]. In BAOCHE subgroup analysis, the point estimates for good functional outcome favored EVT in each of the 6–12 hour (adjusted rate ratio, aRR 1.89 [95% CI 1.15–3.09]) and 12–24 hour (aRR 1.71 [95% CI 1.01–2.90]) windows. In contrast to the anterior circulation late-window trials whereby advanced imaging was utilized to select patients, pc-ASPECTS was adequate for selection of patients into the late window BAOCHE trial, with the majority of patients (approximately two-thirds) selected by non-contrast CT scan and CT angiogram alone. These results support the concept that EVT for late presenting patients with acute BAO has similar efficacy compared to EVT for early presenting patients with BAO or for patients with anterior circulation proximal LVO [30].
As the enrollment window from estimated time of symptom onset was longer for the BAO trials conducted in China, there was less usage of IVT in these trials compared to the BASICS trial. Observational data showed that up to 50% of patients with BAO can achieve mRS 0–3 with mostly IVT treatment if presenting in extended time windows with at least pc-ASPECTS of 8 [31]. This outcome contrasts with that of the MM group in ATTENTION and BAOCHE. Further studies are needed to explore a potential superior recanalization response after IVT in the posterior circulation compared to the anterior circulation. An ongoing trial is testing the efficacy of IVT in patients with BAO in the late time window (NCT05105633). Moreover, whether intra-arterial thrombolysis with urokinase, alteplase, or tenecteplase confers benefit to patients with BAO also remains to be explored, either as primary or adjunctive treatment to mechanical thrombectomy [32-34].
BASICS and BAOCHE included patients with acute BAO and mild symptoms (NIHSS <10) whereas BEST and ATTENTION included only patients with NIHSS ≥10. Including mild strokes in these trials may have diluted the treatment effect of EVT [25]. In our subgroup analysis of patients with low NIHSS, the treatment effect of EVT was not significant. While our analysis was underpowered due to the low sample size, these data, along with the prospective BASICS registry findings, highlights this subgroup of patients as a population that would merit further study to evaluate the benefit of EVT in addition to MM. Management of patients with mild symptoms is challenging as some may improve without EVT while others may deteriorate. The NIHSS also has reduced sensitivity to detect potentially disabling deficits in patients with posterior circulation stroke [35]. Prior studies showed divergent results of EVT in these patients as it carries increased procedural risks, especially in patients with underlying intracranial atherosclerotic disease (ICAD) [12,36,37]. Randomized trials comparing EVT versus MM in BAO patients with mild strokes are warranted.
ICAD, which is considered a potential cause of EVT failure in acute BAO stroke [16,38], was present in approximately 52% of patients in BEST (56% in the EVT group and 49% in the control group) [18], in approximately half of the patients in the ATTENTION trial leading to high rates of intracranial angioplasty +/- stenting (39%) [19], and over half of patients in the BAOCHE trial (intracranial stenting or angioplasty in 54%) [20]. Despite a high frequency of ICAD, a subgroup analysis showed no treatment effect modification based on the presence of ICAD with a significant benefit in ICAD-related LVOs [19]. This is similar to prior studies that showed that, compared to patients without ICAD, patients with ICAD who received rescue treatment achieved similar rates of successful recanalization, favorable outcome, sICH, and mortality at 90 days [16,39].
The rates of sICH were significantly higher in the EVT compared to the control group in all the included BAO trials with rates ranging between 4.5%–8.5% and a pooled rate of 5.4% in the EVT group compared to 0%–1.1% in the control group. These higher rates of sICH could be related to the technical challenges of EVT especially in patients with ICAD who usually require angioplasty and stenting. However, despite the increased rates of sICH, patients treated with EVT had higher odds of favorable outcomes and lower odds of mortality compared to the control group in both the ATTENTION and BAOCHE trials.
The four RCTs included in this meta-analysis were of high quality and low risk of bias. The significant between-studies heterogeneity noted for the primary and secondary outcomes reflects the variation between the four trials especially in terms of inclusion criteria, number of patients, NIHSS thresholds, duration of the study, and different treatment windows. Despite this heterogeneity, the benefit of EVT in acute BAO was demonstrated in this meta-analysis.
There are several limitations in our study. The generalizability of these findings need to be considered as three of the trials were completed in China and Asians are known to have high rates of ICAD [40]. However, as mentioned, prior studies showed that patients with ICAD who received rescue treatment achieved similar rates of successful recanalization and favorable outcome, compared to patients without ICAD [16,39,41]. Data on the percentage of ICAD were not available in the BAOCHE trial and we were unable to compare outcomes of patients with ICAD and without ICAD in this meta-analysis. Further subgroup data of treatment effect by sex, ethnicity, IVT, time window of treatment, pc-ASPECTS, and ICAD would be of interest in a patient-level meta-analysis. Our supplementary meta-analysis for patients with mild BAO (i.e., NIHSS <10) is limited by the fact that BAOCHE only included patients with an NIHSS ≥6. Moreover, the time window in which patients were enrolled between BASICS (6–24 h) and BAOCHE (0–6 h) did not overlap.
Conclusion
This intention-to-treat meta-analysis of the BEST, BASICS, ATTENTION, and BAOCHE trials supports the overall benefit of endovascular treatment in acute BAO up to 24 hours. A treatment effect was not observed in the subgroup of patients with NIHSS <10, although our analysis was underpowered. Further studies are of interest to evaluate the efficacy and safety of EVT in acute basilar occlusion patients presenting with milder symptoms (i.e., NIHSS <10) and the comparison of patients treated with EVT versus IVT.
Notes
Disclosure
The authors have no financial conflicts of interest.