Introduction
Treatment of stroke requires specialized processes that are expediently provided. A multidisciplinary team approach in hospital and effective communication between the stroke team and the emergency medical system (EMS) are prerequisites to a good outcome for patients with acute stroke.1 Multiple specialized processes in stroke management must be streamlined. Information technology plays a key role in modern, complex healthcare. The heavy demands of stroke care could be mitigated to a degree by using information technology. Information technology can reduce the rate of errors, improve communication, make information more readily accessible, assist in diagnosis and monitoring, provide decision support, and enhance implementation of guidelines and recommendations.2
Health-related use of the internet is increasing. As of May 2013, the Pew Internet and American Life Project showed that in the United States, 85% of adults were using the internet, 91% of adults owned a cell phone, 56% of adults owned a smartphone, and 34% owned a tablet device.3 Fifty-two percent of smartphone owners have used their phones to look up health or medical information, and 19% of smartphone owners have downloaded an application specifically to track or manage health. In South Korea, as of July 2012, 78.4% of Koreans were using the internet, 82.3% had a desktop computer, and 63.7% had a smart device (smartphone or tablet computer). Although the internet-use rate has been reported as lower in the elderly population (38.5% of those aged 50-60 years and 9.7% of those aged 60 years or older) than in the younger population, ownership of smart devices is increasing in the former population (46.8% of those 50-60 years old and 23.4% of those aged 60 years or older).4
The World Health Organization has recently defined mobile health as "medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants, and other wireless devices".5 It is anticipated that about 500 million smartphone users around the world will use mobile health services by 2015.6 Mobile devices are increasingly being used to diagnose and treat various diseases. Current mobile devices are particularly suited for medical purposes because of their rich multi-touch user interfaces, built-in accelerometers, location-sensing frameworks, fast processors, and widely available network connections. Additional benefits of mobile devices are that they can be carried easily and can be used anytime and anywhere.7
Here, we address the contribution of information technology and mobile health in the clinical management pathway of stroke patients, particularly regarding their use in the recognition of stroke, transport and triage of stroke patients, emergent stroke evaluation in the hospital, and rehabilitation. We also briefly review the applications of such technology for healthcare providers and patients. However, our intention in this review is not to address in depth all of the information technology issues relating to electronic health records and wearable, ambient monitoring sensors.
Recognition of stroke symptoms
Being aware of stroke warning signs and responding to stroke (calling the emergency services promptly) are two important points in educating the public about stroke. Data show that the public's knowledge of stroke warning signs remains poor worldwide.1 Stroke awareness is also suboptimal in South Korea.8 Several studies demonstrated that use of the EMS was associated with earlier arrival and enabled faster imaging studies.9,10 However, a recent nationwide Korean survey showed that only 33% of respondents chose the proper action of calling the EMS if they exhibited a stroke warning sign.8
The American Heart Association/American Stroke Association guidelines state that activation of the 911 system is strongly recommended (Class I; Level of Evidence B).1 We developed the "stroke 119" (119 being the Korean equivalent to 911) application that provides rapid self-screening for stroke, identifies nearby hospitals that provide thrombolytic treatment, and facilitates calling the EMS.11 This stroke screening tool was adopted from the Cincinnati Prehospital Stroke Scale12 and is displayed in a cartoon format. The multi-touch user interfaces of smartphones enable easy and interactive delivery of information to users. By tapping the cartoon image representing the presence of neurological deficits, the user is informed that he or she may be having a stroke and is given instructions to call the EMS. A global positioning system, which is a built-in function of smartphones, enables users to determine their location and search for nearby hospitals. This helps stroke victims, witnesses, and EMS personnel find nearby hospitals that provide acute stroke care in real time. Thus, the stroke 119 application is useful for reducing hospital arrival times for thrombolytic patients. Similarly, the American Stroke Association recently developed the "Spot a Stroke F.A.S.T." application. The F.A.S.T. provides users with an easy way to remember the sudden signs of stroke and to find a nearby hospital.13 Wide adoption of applications that improve recognition of stroke symptoms might be associated with getting stroke victims to the hospital more quickly.
Transport and triage of stroke patients
Remote assessment of stroke patients
Telemedicine is the use of information and communication technology to provide healthcare services to individuals who are at a distance from the healthcare provider.14 Patients in remote areas who suffer from stroke can gain access to timely expert care by stroke specialists via telemedicine.15 This may be particularly useful in underserved or rural areas. Because telestroke consultations require high-speed, clear, and reliable audio-video data transmission to ensure adequate neurological evaluation, typical telemedicine systems are expensive.15 With recent advances in one-way/two-way video and teleradiology features adapted to smartphones, several investigators have reported the efficacy of ubiquitous and relatively cheap mobile-device-based telemedicine.16,17 Mobile telemedicine systems can be freely used while at work and home as well as while traveling via a wireless internet service and a smartphone.
National Institutes of Health Stroke Scale telestroke examination
Because mobile devices can deliver streaming video and audio, they can be used to evaluate acute stroke patients remotely.18 Comparison between the face-to-face method and the mobile telemedicine method of assessment using the National Institutes of Health Stroke Scale (NIHSS) showed high inter-method agreement according to the correlations in total NIHSS scores between the methods (r=0.94 to 0.98, P<0.001) and an acceptable length of remote assessment time (3.38 to 11.4 minutes).15 Therefore, current guidelines state that the NIHSS telestroke examination, when administered by a stroke specialist using high-quality videoconferencing, is recommended when an NIHSS bedside assessment by a stroke specialist is not immediately available for patients with acute stroke (Class I; Level of Evidence A).19
Teleradiology
Teleradiology is a critical aspect of telestroke assessment and is defined as obtaining radiographic images at one location and transmitting them to another for diagnostic and consultative purposes.20 Several investigators have shown that the smartphone-based client-server teleradiology system may have the potential to allow urgent management decisions in acute stroke.21,22 Using a telestroke network, the agreement on identification of contraindications for thrombolytic treatments in noncontrast CT was excellent between vascular neurologists who used a smartphone application and radiologists who used desktops in a hospital.16 Recent guidelines indicate that the teleradiology systems approved by the Food and Drug Administration or equivalent organization are useful in supporting rapid imaging interpretation in time for making decisions on thrombolytic treatment when implemented within a telestroke network (Class I; Level of Evidence B).1
Prehospital notification system
Previous studies showed that only 15-60% of patients with stroke arrived at the hospital within three hours after the onset of symptoms, and only 14-48% arrived within two hours.23 Moreover, the proportion of patients with ischemic stroke who arrived within two hours of symptom onset did not increase significantly from 2003 to 2009.24
Prenotification of a stroke patient's arrival by EMS personnel can shorten the time before the patient is seen for initial evaluation by a physician in the emergency department, shorten the time to brain imaging, and increase the use of IV recombinant tissue plasminogen activator (rt-PA).10,25,26 Thus, prehospital notification is recommended in current guidelines in the United States and Europe.1,27 EMS prenotification, including time of symptom onset or potential contraindications for rt-PA, facilitates earlier activation of a stroke team and the preparation of imaging modalities before the patient arrives.23 The Get With the Guidelines-Stroke program found that, compared with patients who arrived without prenotification, patients who arrived with prenotification had shorter door-to-imaging times, door-to-needle times, symptom-onset-to-needle times, and a greater likelihood of treatment with rt-PA within three hours. Despite these benefits, EMS prenotification occurred in only two-thirds of patients with acute ischemic stroke arriving by EMS.28
In contrast to telemedical communication between two hospitals, telemedical transmission from the ambulance in the field to the stroke center is still a challenge. German researchers tested the feasibility of telemedicine-equipped ambulances. Among 18 of the 30 scenarios the NIHSS assessment could not be performed due to absence or loss of the audio-video signal. Moreover, the remaining 12 completed scenarios did not meet an acceptable level for clinical use.29 In the actual stroke patients, telemedically assisted prehospital care and regular EMS care were compared, but the researchers found that system dropouts occurred in three out of 18 missions. Moreover, there was no decrease in time intervals or improvement in diagnostic accuracy.30 Thus, although prehospital consultation has the potential to improve emergency care, especially when no highly trained personnel are on-scene,31 insufficient reliability of telemedicine technologies resulting from temporary dropouts and local unavailability of mobile networks is still an unresolved problem that limits their use in clinical practice. Therefore, further technical development is needed in prehospital notification systems. As an intermediate step, communication using personal digital assistants or smartphones was tested.32,33 Although many developing countries do not have widespread or even dependable broadband internet access, much of their population can access the internet using cell phones.5 In this respect, prenotification using mobile devices, especially where the internet connection is limited, might be promising.
Mobile stroke unit
The mobile stroke unit is equipped with a CT scanner, a point-of-care laboratory, and a telemedicine connection to the hospital. A randomized trial of the mobile stroke unit strategy demonstrated that its prehospital stroke treatment could reduce the median time from alarm to treatment decision from 76 to 35 minutes (median difference of 41 minutes, P<0.0001). The mobile stroke unit strategy seems to bring guideline-adherent stroke treatment directly to the emergency site, thus speeding up acute stroke management considerably.34
Emergent stroke evaluation in the hospital
In patients eligible for IV rt-PA, the benefit of treatment is time-dependent, and treatment should be initiated as quickly as possible.35 For every 15-minute reduction in door-to-needle time, the odds of risk-adjusted in-hospital mortality were reduced by 5%.36 The door-to-needle time should be within 60 minutes from hospital arrival (Class I; Level of Evidence A).1 Nevertheless, The Get With The Guidelines-Stroke data showed that only 26.6% of patients had a door-to-needle time within 60 minutes among the 25,504 acute ischemic stroke patients treated at 1,082 hospital sites in the United States.36
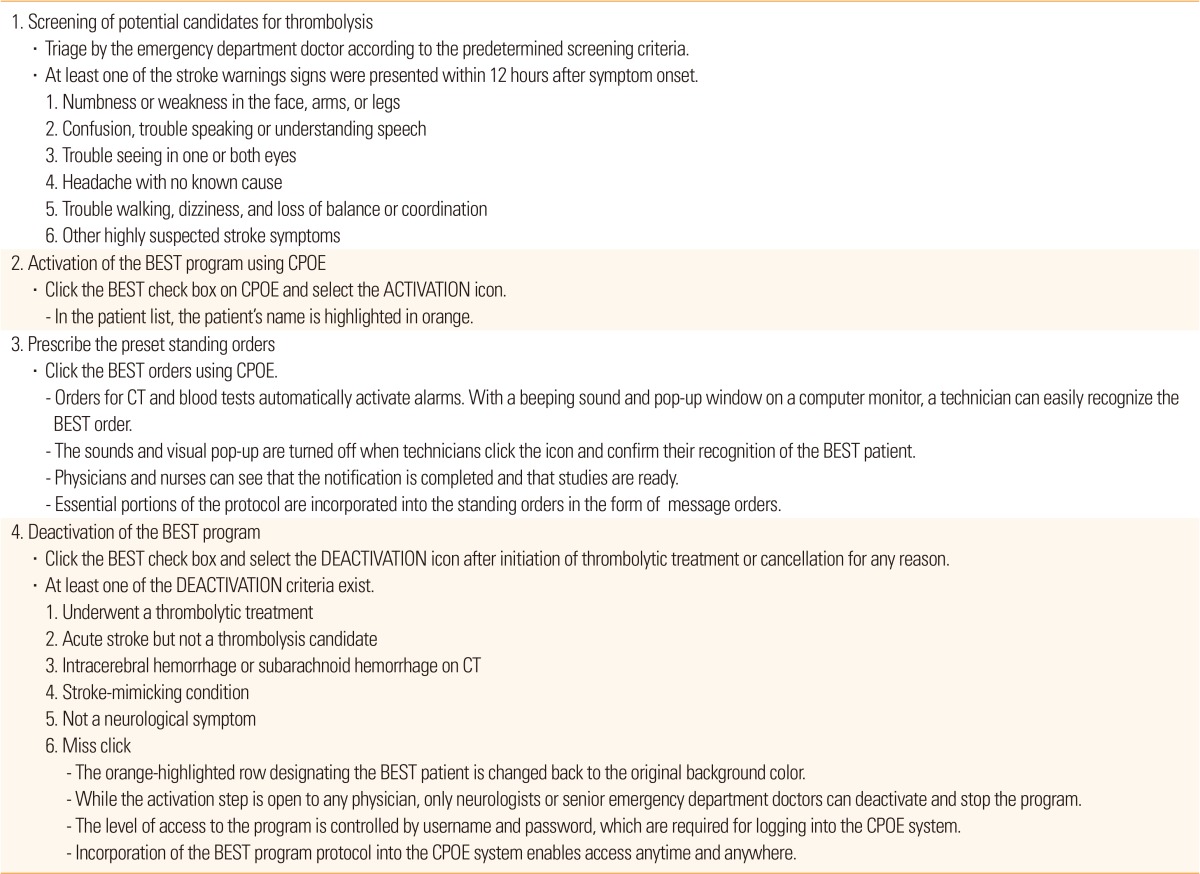
Within hospitals, established protocols are beneficial to optimize medical processes. Incorporation of protocols into a computerized physician-order entry can enhance communication among team members.37 Shortening door-to-needle time requires rapid triage, notification, and action by many medical staff members in different departments, including the emergency, neurology, nursing, neuroimaging, and laboratory departments. Notification by phone to different medical staff members and technicians takes time. Single-call systems to activate all stroke-team members can reduce door-to-needle times in patients with acute ischemic stroke.38 Using information technology rather than a pager can be more effective for communication between stroke-team members because notification can be done simultaneously. It is also possible to use a predetermined order set and monitor time logs by easily acquiring time data for individual evaluation and treatment steps through the use of information technology. A computerized in-hospital alert system, which uses a computerized physician order entry, was developed and shown to be effective in a single medical center (Table 1).39 The effect of this system was also demonstrated in a multicenter study with various hospital settings.40 A computerized in-hospital alert system may be the impetus for healthcare providers to improve multidisciplinary care delivery and patient care quality.41
Mobile devices as supplementary tools for neurologic examination and decision making
A mobile-device-supported neurological examination
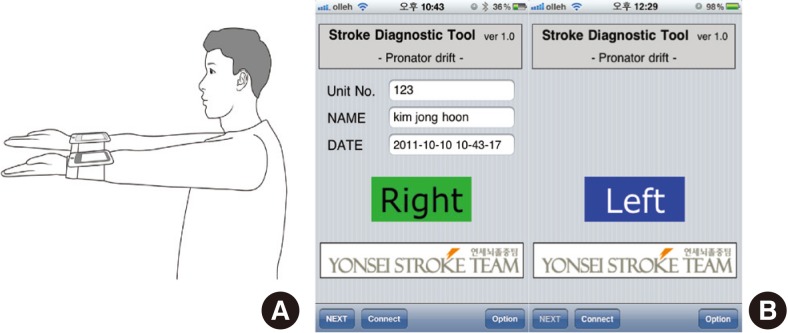
Portable mobile devices have been used to easily administer neurological examinations, including measuring visual acuity and color vision.42 Because mobile devices have rich multitouch user interfaces and built-in accelerometers,42 these features might be useful for assessing patients' neurologic deficits. The pronator drift test is a neurologic examination used to evaluate mild arm weakness. The presence or absence of pronation and drift are determined qualitatively. Several studies have demonstrated that accelerometers are reliable tools for quantifying physical activity and walking speed after stroke.43,44 We developed the "iPronator" application to objectify the pronator drift test using a built-in accelerometer on mobile devices.45,46 The iPronator measures changes in the x- and y-axes that correspond to pronation and drift, respectively. A Bluetooth connection between mobile devices on each arm enables data transfer in real time (Figure 1). We found that the parameters of pronation (average and maximum) and drift (average, maximum and oscillation) were significantly different between patients and healthy controls. The iPronator application was also useful for determining degrees of improvement in patients with arm weakness by providing quantitative data for serial tests.
Decision making support for stroke classification
Reports indicate that physicians have difficulty processing complex information.47 The use of information technology can support decision making by providing installation of preprogrammed algorithms and an easily accessible user interface. Classification of stroke subtypes is based on a logical algorithm. Therefore, information technology can be effectively used for accurate classification of stroke subtypes.
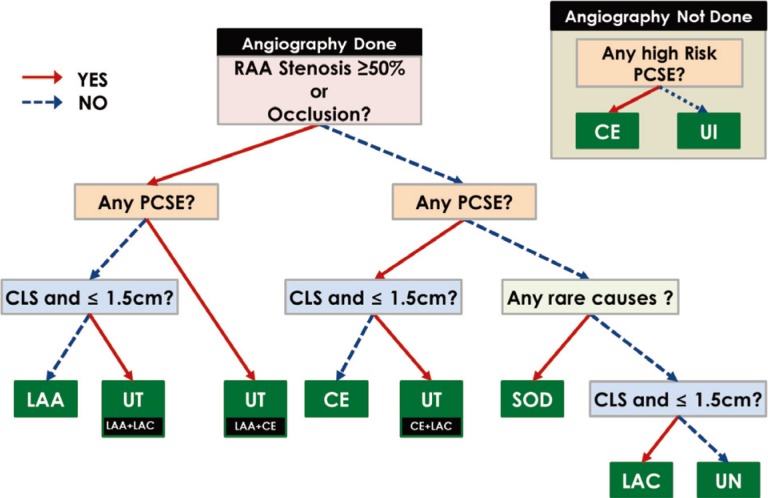
The Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification is a widely used classification system of ischemic stroke that primarily utilizes the etiology of strokes for classification.48 However, the inter-rater reliability of the TOAST classification is known to be modest. To overcome the limitations of TOAST classification, several computerized classification systems have been developed. Goldstein et al. reported that a computerized algorithm and standardization of procedures for extracting medical records could improve both intraobserver and interobserver agreement.49 The Causative Classification System50 and the Atherosclerosis-Small Vessel Disease-Cardiac Source-Other Cause classification system showed good-to-excellent agreement in comparison with the original TOAST scheme.51
Although these computerized classification systems showed excellent agreement among raters, they usually run through desktop internet web pages, which may limit their wide use in practice. Thus, we developed a computerized clinical-decision support system running on mobile devices and named it "iTOAST".7,52 A logical algorithm of the TOAST classification system was analyzed and implemented (Figure 2). After answering questions using the touch interface, the results of the stroke subtype are displayed on the screen. We found that the inter-rater agreement was higher when the raters used iTOAST (0.790, 95% CI: 0.707-0.870) than the conventional method (0.692 , 95% CI: 0.600-0.782; P<0.001). Thus, the iTOAST was easier, more accurate, and more reliable than the conventional method, and it has the additional benefit of accessibility because it runs on a mobile device. Decision-making support in stroke management is also promising for emergent situations. A pilot application of "i-Stroke" had successful information transfer, allowing medical staff to discuss stroke patients' diagnosis and management.17
Rehabilitation
Virtual reality
Virtual reality (VR) is a new type of rehabilitation therapy that can be used with handicapped patients with stroke. Typically, VR systems include computer-based programs designed to simulate real-life objects and events.53 VR systems give sensory feedback to patients, in most cases visual or audio feedback, which can improve patients' cognitive and motor functions. Several studies have shown that VR is beneficial to arm function,54,55 walking,56 and neglect.57,58 However, the Cochrane review stated that there was insufficient evidence for any conclusion on the effectiveness of VR on grip strength or gait speed. It is also unclear at present which characteristics of VR are most important, and it is unknown whether the effects can be sustained in the long term.53 However, VR may be advantageous because it offers a number of unique features. For instance, goal-oriented tasks and repetition of said tasks are important in neurological rehabilitation; VR can encourage repetition of tasks by providing simulated real-life functional activities, which are more interesting and enjoyable for both children and adults. Moreover, activities that are unsafe to practice in the real world, such as crossing the street, driving, or preparing food, can be trained with VR. Furthermore, tasks can be graded and immediate feedback can be provided. Many VR programs are designed to be used without supervision.53
Telerehabilitation
Telerehabilitation can offer prolonged rehabilitation for patients with stroke after they are discharged from the hospital.59 Telerehabilitation allows the patient to maintain contact with medical professionals, doctors, and therapists in a comfortable home environment, while also enabling continuation of long-term rehabilitation to promote functional abilitites. Furthermore, telediagnostics enable transmission of messages and monitoring of patient outcomes and functional progress, as well as changes in the rehabilitation strategy and planning of outpatient visits. Numerous studies clearly show that telerehabilitation improves functional performance and quality of life as well as increases patient satisfaction.60,61 In the near future, telerehabilitation and VR may be among the major advanced technologies in post-stroke rehabilitation for the assessment and management of patients.
Delivery of medical information to healthcare providers and the general population
Applications for healthcare providers
Transient symptoms of stroke patients can be easily captured by caregivers or healthcare professionals onsite and then reported to stroke experts using mobile devices. Furthermore, smartphones are used to calculate medical formulas, find drug references, search literature, and access medical education/training. Healthcare providers can also use smartphones in the diagnosis and objectification of neurological symptoms45 and to obtain support for clinical decisions.7
As compared with paper guidelines, computer-based guidelines running on a mobile device can improve diagnostic decision making for pulmonary embolisms.62 The Clinical Research Center for Stroke in South Korea provides a smartphone application for stroke guidelines.63 This smartphone application can be useful in daily clinical practice because it is accessible anytime and anywhere. Providing timely updates on guidelines is another advantage of this application; readily available updates to guidelines can help physicians better adhere to evidence-based medicine. In addition, mobile applications can be helpful in clinical trials for pre-screening, assessment of eligibility, and randomization of patients.64
Applications for patients
Self-management and remote monitoring of patients are becoming viable solutions for management of diseases with chronic conditions, including stroke. The risk of stroke is as high as 12.8% during the first week after a transient ischemic attack. At least 80% of recurrent events might be prevented with the use of a comprehensive approach.65 To prevent stroke recurrence, drug compliance, risk-factor control, and lifestyle modification are important.
Cell phone messaging interventions can serve as preventive measures by improving patients' health status and behavior.66 Indeed, the delivery of stroke warning signs through text messages is one way to get people thinking about the dangers of stroke.67 Furthermore, smartphone applications will doubtlessly play an important role in the future in patient education, self-management, and remote monitoring.68 Lifestyle applications can help manage weight control, diet and cooking, and exercise. The Clinical Research Center for Stroke in South Korea has developed the "Stroke STOP" application, which provides risk-factor-control tools, medication reminders, and public information about stroke.69
Comments
Information technology and smart devices can be useful in many aspects of stroke management, which may improve patient outcomes. Greater automation of a hospital's information system resulted in fewer complications, lower mortality rates, and lower costs. Furthermore, information technology using smart devices, including smartphones and tablet computers, will be a cornerstone of good clinical care in hospital environments. Although there are now hundreds of applications focusing on wellness, fitness, and nutrition for the general population, the development of healthcare applications for stroke patients will provide more opportunities to improve stroke management. However, many applications are developed by programmers without the involvement of doctors or patients. Thus, participation of stroke healthcare professionals in the design of mobile applications would be beneficial to their development and implementation.