Endovascular Therapy in the Extended Time Window for Large Vessel Occlusion in Patients With Pre-Stroke Disability
Article information
Abstract
Background and Purpose
We compared the outcomes of endovascular therapy (EVT) in an extended time window in patients with large-vessel occlusion (LVO) between patients with and without pre-stroke disability.
Methods
In this prespecified analysis of the multinational CT for Late Endovascular Reperfusion study (66 participating sites, 10 countries between 2014 and 2022), we analyzed data from patients with acute ischemic stroke with a pre-stroke modified Rankin Scale (mRS) score of 0–4 and LVO who underwent EVT 6–24 hours from the time last seen well. The primary outcome was the composite of functional independence (FI; mRS score 0–2) or return to the pre-stroke mRS score (return of Rankin, RoR) at 90 days. Outcomes were compared between patients with pre-stroke disability (pre-stroke mRS score 2–4) and those without (mRS score 0–1).
Results
A total of 2,231 patients (median age, 72 years; median National Institutes of Health Stroke Scale score, 16) were included in the present analysis. Of these, 564 (25%) had pre-stroke disability. The primary outcome (FI or RoR) was observed in 30.7% of patients with pre-stroke disability (FI, 16.5%; RoR, 30.7%) compared to 44.1% of patients without (FI, 44.1%; RoR, 13.0%) (P<0.001). In multivariable logistic regression analysis with inverse probability of treatment weighting, pre-stroke disability was not associated with significantly lower odds of achieving FI or RoR (adjusted odds ratio 0.73, 95% confidence interval 0.43–1.25). Symptomatic intracranial hemorrhage occurred in 6.3% of both groups (P=0.995).
Conclusion
A considerable proportion of patients with late-presenting LVO and pre-stroke disability regained pre-stroke mRS scores after EVT. EVT may be appropriate for patients with pre-stroke disability presenting in the extended time window.
Introduction
Research on the development of evidence-based recommendations for endovascular treatment (EVT) of large-vessel occlusion (LVO) stroke in patients with pre-stroke disability is limited. Current guidelines recommend EVT for acute ischemic stroke in cases with a pre-stroke modified Rankin Scale (mRS) score of 0–1 [1,2]. However, more than one-third of patients presenting with ischemic stroke have a pre-stroke disability [3]. These patients were excluded from most trials [4-8]. There is no clear pathophysiological reason to withhold EVT from patients with pre-stroke disability who are otherwise eligible for and may benefit from intervention [9]. Considering the strong efficacy of EVT in acute ischemic stroke [4-8,10], it is important to determine whether patients with pre-existing disability can benefit from thrombectomy [11,12].
For stroke presenting in the early time window (0–6 hours from time last seen well [TLSW]), several observational studies compared outcomes after EVT between patients with and without pre-stroke disability [13-17]. These studies included no worsening of the mRS score at 90 days post-stroke as the primary outcome, distinct from the commonly used outcome measure of functional independence (mRS score 0–2) at 90 days [18]. When using this outcome measure, EVT outcomes were not necessarily worse in patients with pre-stroke disability compared to those without [13-17]. Furthermore, a sub-analysis of Japanese registry data suggested that endovascular management for anterior circulation LVO is more likely to lead to better functional outcomes at 90 days than medical therapy, mainly in cases of early stroke [19]. A recent analysis of the CT for Late Endovascular Reperfusion (CLEAR) study revealed similar results in late anterior circulation stroke 6–24 hours after TLSW [20]. Because selection bias affects outcomes when comparing treatments in observational studies, it is important to study functional outcomes after EVT for late stroke in patients with and without pre-stroke disability. Moreover, considering that approximately one-third of patients with acute LVO stroke present in the late time window [21], there is a paucity of evidence on the effectiveness of EVT in late stroke compared to that in early stroke in patients with pre-existing disability.
Even in an extended time window, patients with LVO stroke with pre-stroke disability possibly do not have a worse functional prognosis than those without pre-stroke disability considering their pre-stroke mRS score; however, this hypothesis has not been investigated. In this analysis of the CLEAR study [20,22,23], we aimed to evaluate the clinical outcomes and safety of EVT for late-presentation stroke in patients with and without pre-stroke disability.
Methods
The senior author (T.N.N.) and lead statistician (M.M.Q.) had access to all the study data. This study was conducted according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [24]. Anonymized data are available from the corresponding author upon reasonable request.
This was an investigator-initiated study. The funder had no role in the study design, analysis, management, or writing. Approval from the local institutional review board or ethics committee was obtained from all participating sites. The requirement for written informed consent was waived because of the retrospective nature of this study and because the research was considered to pose no more than minimal risk to the subjects.
Study population
This study was conducted as a pre-specified analysis of the CLEAR registry (NCT04096248). CLEAR is an international, multicenter, retrospective study comparing outcomes of patients with LVO stroke presenting in the late window (6 to 24 hours) for whom the treatment strategy was selected by either non-contrast computed tomography (CT) only or advanced imaging with CT perfusion or magnetic resonance imaging [20,22,23,25-27]. Data of patients with acute ischemic stroke with LVO presenting 6–24 hours after TLSW and with an Alberta Stroke Program Early CT Score (ASPECTS) of ≥5 were collected from 66 sites in 10 countries (United States, Belgium, Canada, Finland, France, Germany, Japan, Portugal, Spain, and Switzerland) between January 2014 and May 2022.
Consecutive patients from the CLEAR study were eligible for the present analysis if they met the following inclusion criteria: (1) a baseline National Institutes of Health Stroke Scale (NIHSS) score of ≥6; (2) occlusion of the internal carotid artery, proximal middle cerebral artery (MCA) (M1/M2 segments), or basilar artery; (3) a pre-stroke mRS score of 0–4; (4) a time from TLSW to treatment of 6–24 hours; and (5) patients who underwent EVT. Patients without information on pre-stroke or 90-day mRS scores were excluded from the analysis. The pre-stroke mRS score was assessed on admission by a stroke-trained physician with experience in using the mRS, according to the following scale: 0=no symptoms at all; 1=no significant disability despite symptoms, able to carry out all usual duties and activities; 2=slight disability, unable to carry out all previous activities but able to look after own affairs without assistance; 3=moderate disability, requiring some help, but able to walk without assistance; 4=moderately severe disability, unable to walk without assistance, and unable to attend to own bodily needs without assistance; and 5=severe disability, bedridden, incontinent, and requiring constant nursing care and attention [28].
Outcomes
The primary outcome was the composite of functional independence (FI; mRS score 0–2) or return to pre-stroke mRS score (return of Rankin, RoR) at 90 days [20]. Secondary outcomes were RoR at 90 days, utility weighted (UW)-mRS score at 90 days, mean change in UW-mRS score (mean UW-mRS score at 90 days minus pre-stroke UW-mRS score), symptomatic intracranial hemorrhage (defined as a 4-point worsening in the NIHSS attributed to an intracranial hemorrhage) [29], mortality at 90 days, and severe disability or mortality (mRS score 5–6) at 90 days. UW-mRS scores were derived from the DAWN trial, with 10.0, 9.1, 7.6, 6.5, 3.3, 0, and 0 assigned to mRS scores of 0, 1, 2, 3, 4, 5, and 6, respectively [5,30]. The UW-mRS score was included among the secondary outcomes given the minimal difference in disability between scores of 0, 1, and 2 compared with the considerable disability in patients with scores ≥3, with expected ceiling effects observed among patients with markedly low pre-stroke mRS scores (e.g., patients with a pre-stroke mRS score of 0 or 1 are likely to do well with EVT but are unlikely to return to an mRS score of 0 or 1 at 90 days). A standard approach to mRS assessment was used [22].
Statistical analysis
The Mann–Whitney U test for continuous and ordinal variables and the Pearson χ2 test for categorical variables were used to compare patient groups. We further compared the outcomes between patients with pre-stroke disability (pre-stroke mRS score 2–4) and those without (pre-stroke mRS score 0–1) using univariable and multivariable logistic regression models accounting for clustering by site with a logit link function and binomial distribution specifications [14,15,17]. Crude and adjusted odds ratios (OR) with 95% confidence intervals (CI) were computed.
We used the propensity score-based inverse probability of treatment weighting (IPTW) method to account for confounding factors. Using the IPTW, we estimated the average treatment effect (the effect of pre-stroke disability on the entire population with pre-stroke disability vs. the entire population without pre-stroke disability). The following covariates were included a priori in the multivariable model and IPTW: age, sex, baseline NIHSS score, atrial fibrillation, intravenous thrombolysis, ASPECTS, occlusion location (internal carotid vs. MCA-M1 vs. MCA-M2 vs. basilar artery), and time from TLSW to treatment. The model was fitted using PROC GENMOD in SAS 9.4 (SAS Institute, Cary, NC, USA) with a logit link function and binomial distribution specifications.
In all analyses, a generalized estimating equation accounted for clustering by site. An independent correlation structure with the smallest quasi-likelihood independence criterion value was assumed for the within-site clustering of patients. Statistical analyses were performed using SAS version 9.4. All tests were twosided, and a P value less than 0.05 was considered significant.
Sensitivity analyses
The following sensitivity analyses were performed: (1) evaluation of FI or RoR at 90 days in the anterior circulation subgroup only, excluding patients with basilar artery occlusion; (2) evaluation in the subgroup excluding patients whose mRS score improved from pre-stroke to 90 days; (3) addition of hypertension and diabetes to the pre-specified covariates using the complete case dataset; and (4) addition of hypertension, diabetes, transfer, and imaging modalities to the pre-specified covariates using the complete case dataset. Furthermore, we performed analyses excluding patients with a pre-stroke mRS score of 2.
Missing data analysis
In addition to performing analysis on patients with all available data (complete case analysis), we repeated the analysis after imputing data values for the missing covariates, ASPECTS, atrial fibrillation, and intravenous thrombolysis. Missing data were correlated with several covariates (data not presented in the tables); therefore, a missing at random mechanism was assumed. Multiple imputations were performed in SAS 9.4 using PROC MI, and 20 imputed datasets were generated. A fully conditional specification method was applied. PROC MIANALYZE was used to pool results from the logistic regression analysis performed on the 20 imputed datasets and to generate pooled ORs and 95% CI.
Results
Patients
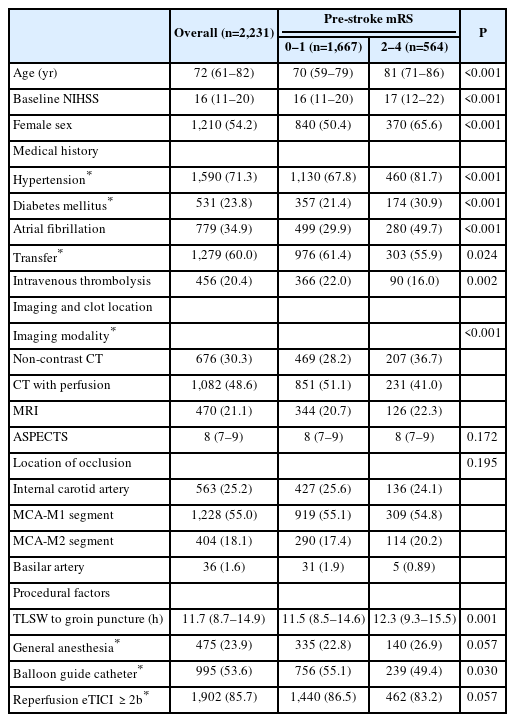
Of the 5,098 patients enrolled in the CLEAR study, 2,533 met the eligibility criteria for the current study, and 2,231 were included in the analysis after excluding 302 patients with missing covariates (Figure 1). The median (interquartile range, IQR) age of the cohort was 72 (61–82) years, with a median NIHSS score of 16 (11–20), and most occlusions occurred in the M1 segment of the MCA (55.0%). Reperfusion of expanded Thrombolysis In Cerebral Infarction (eTICI) ≥2b was achieved in 85.7% of patients (Table 1). The pre-stroke mRS scores were as follows: 0 (n=1,286), 1 (n=381), 2 (n=269), 3 (n=200), and 4 (n=95). Pre-stroke disability (mRS score 2–4) was observed in 564 (25%) patients, and a lack of pre-stroke disability (mRS score 0–1) was observed in 1,667 (75%) patients.
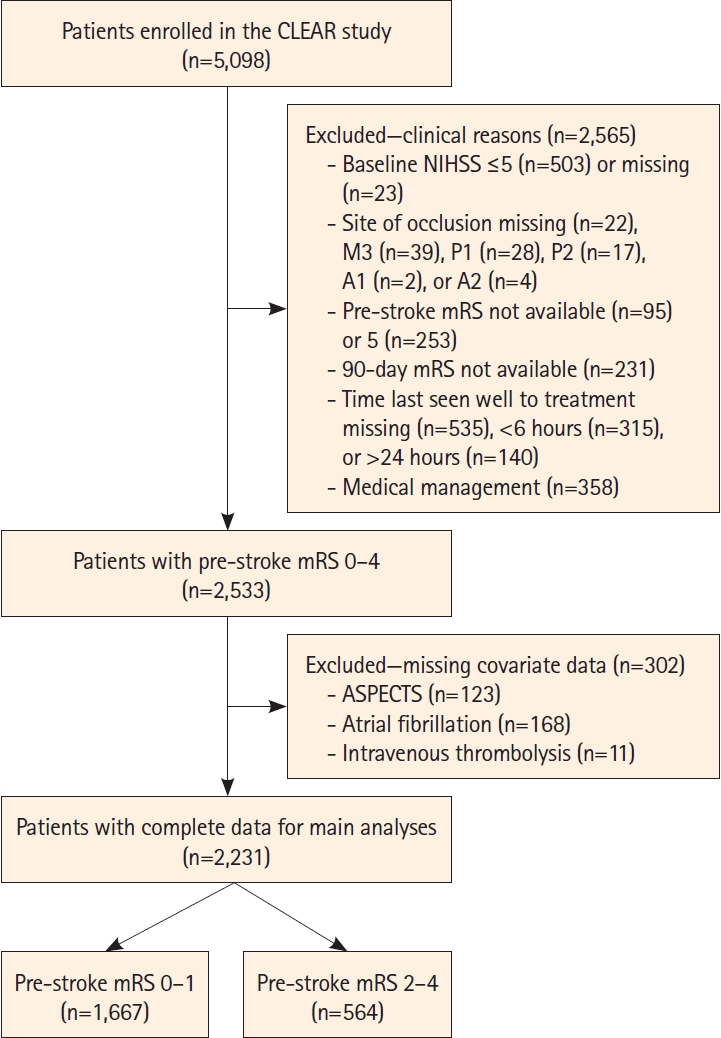
Flow diagram of patient selection. CLEAR, CT for Late Endovascular Reperfusion; NIHSS, National Institutes of Health Stroke Scale; mRS, modified Rankin Scale; ASPECTS, Alberta Stroke Program Early CT Score.
Compared to patients without pre-stroke disability, patients with pre-stroke disability were older (median age [IQR], 81 [71–86] vs. 70 [59–79] years, P<0.001); had higher baseline NIHSS (median [IQR], 17 [12–22] vs. 16 [11–20], P<0.001); had higher frequency of hypertension, diabetes mellitus, and atrial fibrillation (P<0.001 each); were transferred from primary care centers to thrombectomy centers less often (55.9% vs. 61.4%, P=0.024); and received intravenous thrombolysis less frequently (16% vs. 22%, P=0.002). Patients with pre-stroke disability had a longer time from TLSW to groin puncture (median [IQR], 12.3 [9.3–15.5] vs. 11.5 [8.5–14.6] hours, P=0.001), while treatment selection with non-contrast CT was more common (36.7% vs. 28.2%, P<0.001) than that in patients without pre-stroke disability. Within the subgroup of patients transported directly to EVT centers (39.9% of the total [852/2,131]), the time from hospital arrival to groin puncture showed no significant difference between patients with (median [IQR], 91 [69–126] minutes, n=239) and those without pre-stroke disability (90.5 [65–123] minutes, n=613) (P=0.50). Balloon guide catheter use was less common in patients with pre-stroke disability than in those without (49.4% vs. 55.1%, P=0.03), and inter-group difference in the rate of achieving eTICI ≥2b reperfusion was not significant (83.2% vs. 86.5%, respectively, P=0.057) (Table 1).
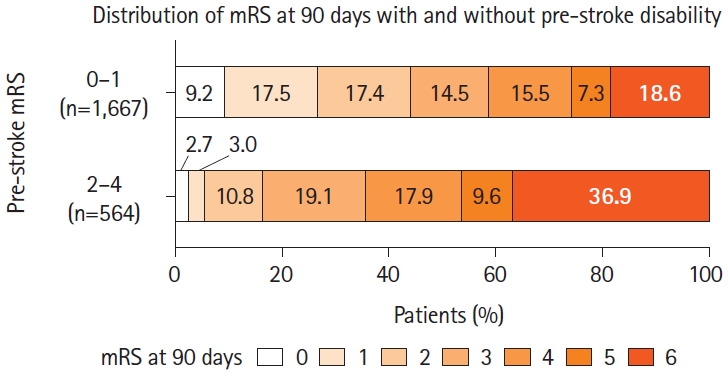
The distribution of mRS scores at 90 days according to the prestroke mRS score is shown in Figure 2. The mRS score at 90 days tended to be higher in patients with a pre-stroke mRS score of 2–4 than that in patients with a pre-stroke mRS score of 0–1. The 90-day mRS score was lower than the pre-stroke mRS score in 3.1% (70/2,231) overall, 3.7% (14/381) in patients with a pre-stroke mRS score of 1, 5.6% (15/269) in patients with a pre-stroke mRS score of 2, 6.0% (12/200) in patients with a pre-stroke mRS score of 3, and 30.5% (29/95) in patients with a pre-stroke mRS score of 4 (Supplementary Figure 1).
Primary outcome
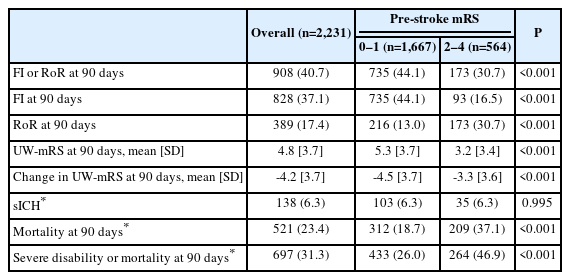
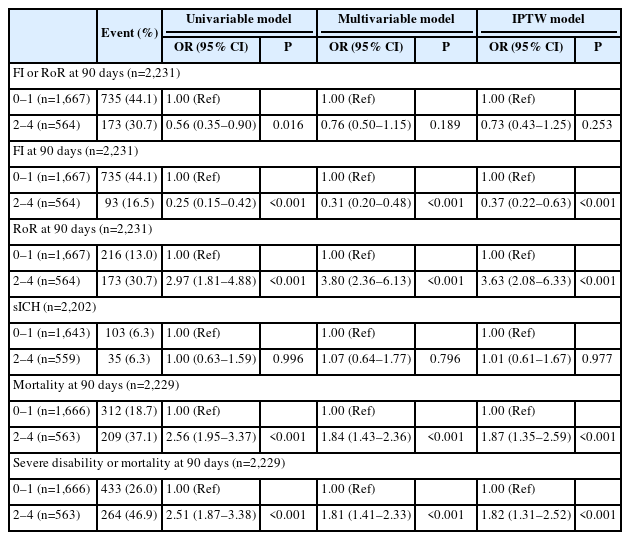
The primary outcome (FI or RoR) was observed in 30.7% of patients with pre-stroke disability (FI, 16.5%; RoR, 30.7%) and 44.1% of patients without (FI, 44.1%; RoR, 13.0%) (P<0.001) (Table 2). In the pre-stroke disability group, FI or RoR was achieved in 24.9% (FI, 15.6%; RoR, 24.9%) of patients with a pre-stroke mRS score of 2–3 (n=469) and 58.9% (FI, 21.1%; RoR, 58.9%) of patients with a pre-stroke mRS score of 4 (n=95). In both multivariable logistic regression and IPTW analyses, pre-stroke disability was not associated with lower odds of achieving FI or RoR (adjusted odds ratio [aOR] 0.76, 95% CI 0.50–1.15 and aOR 0.73, 95% CI 0.43–1.25) (Table 3). In sensitivity analyses, pre-stroke disability was not associated with lower odds of FI or RoR excluding patients with basilar artery occlusion (IPTW: aOR 0.75, 95% CI 0.44–1.29), adding hypertension and diabetes to the pre-specified multivariable model (IPTW: aOR 0.73, 95% CI 0.42–1.24), or adding hypertension, diabetes, transfer, and imaging modality to the pre-specified model (IPTW: aOR 0.69, 95% CI 0.41–1.17). The sensitivity analysis of the subgroup excluding patients whose mRS score improved at 90 days showed significantly lower odds of FI or RoR in patients with pre-stroke disability compared to those without (IPTW: aOR 0.51, 95% CI 0.39–0.66) (Supplementary Table 1). The analysis excluding patients with a pre-stroke mRS score of 2 showed no significant reduction in the odds of FI or RoR in the pre-stroke mRS 3–4 disability group compared with patients without pre-stroke disability (IPTW: aOR 0.94, 95% CI 0.40–2.22) (Supplementary Table 2). The reduction in the odds of RoR or FI in patients with pre-stroke disability compared to those without was not significant in the analysis with imputation of missing data (IPTW: aOR 0.76, 95% CI 0.45–1.28) (Supplementary Table 3).
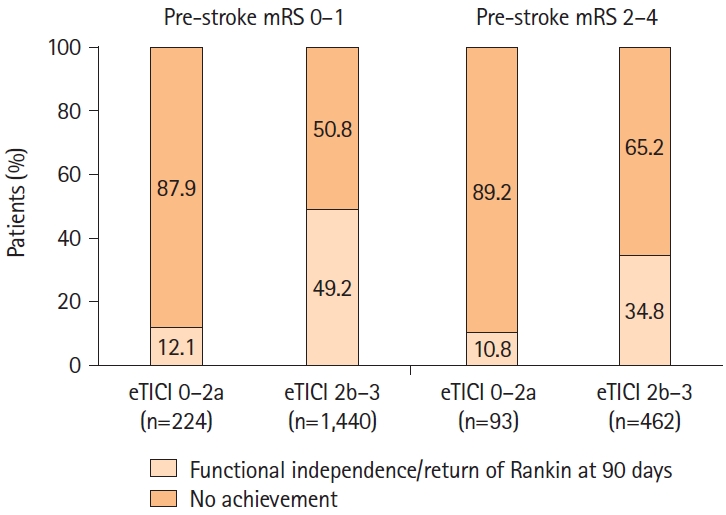
FI or RoR was achieved in a significantly higher percentage of cases in patients with eTICI ≥2b reperfusion than in patients with eTICI 0–2a in patients without pre-stroke disability (49.2% vs. 12.1%, P<0.001) and in those with pre-stroke disability (34.8% vs. 10.8%, P<0.001) (Figure 3).
Secondary outcomes
Patients with pre-stroke disability had significantly less FI (IPTW: aOR 0.37, 95% CI 0.22–0.63) but significantly more RoR (IPTW: aOR 3.63, 95% CI 2.08–6.33) at 90 days than those without pre-stroke disability (Table 3). Consistent with this observation, the UW-mRS score at 90 days was significantly lower in patients with pre-stroke disability (mean [standard deviation, SD] 3.2 [3.4] vs. 5.3 [3.7], P<0.001); however, the magnitude of change in the UW-mRS score at 90 days was smaller than that in patients without pre-stroke disability (mean change [SD] -3.3 [3.6] vs. -4.5 [3.7], P<0.001). In both groups, sICH was seen in 6.3% (IPTW: aOR 1.01, 95% CI 0.61–1.67) (Tables 2 and 3). Both mortality and severe disability or mortality at 90 days were significantly increased in patients with pre-stroke disability compared to those without pre-stroke disability (IPTW: aOR 1.87, 95% CI 1.35–2.59; aOR 1.82, 95% CI 1.31–2.52, respectively) (Table 3). In the analysis with imputation of missing data, the odds ratios of sICH, mortality, and severe disability or mortality were similar to those in the models of the main analysis (Supplementary Table 3).
Discussion
In this pre-specified analysis of the CLEAR study, outcomes after EVT for acute large-vessel stroke in the predominantly anterior circulation 6–24 hours after TLSW showed comparable improvement for patients with pre-stroke disability (pre-stroke mRS score of 2–4) and those without (pre-stroke mRS score 0–1). In accordance with previous reports, the achievement of FI or RoR at 90 days was selected as the primary outcome to allow for observations reflecting the severity of the patient’s baseline disability [13-17,19,20]. As expected, the achievement of FI or RoR was numerically lower in patients with pre-stroke disability than in patients without. However, after adjusting for confounders, the multivariable and IPTW models did not show a significant difference between the two groups in the likelihood of achieving this primary outcome measure.
In this study, FI or RoR was achieved in 30.7% of patients with pre-stroke disability after EVT for late LVO stroke. In previous reports of early presentation stroke, the rates of FI or RoR after EVT for anterior circulation large vessel stroke with a pre-stroke mRS score of ≥2 ranged from 26.7% to 37.7% [13-15,17]. Patients in these studies had early presentation stroke. The present study suggests that even in patients with late-presenting large-vessel stroke, the proportion of patients with pre-stroke disability who achieve FI or RoR after EVT, that is, the proportion of patients whose disability does not increase as measured by the mRS, is similar to that in patients who present with early stroke.
In the present analysis, the achievement rate of FI or RoR was significantly greater in cases with successful reperfusion than that in cases without successful reperfusion in patients with and without pre-stroke disability, suggesting that successful reperfusion with interventions including EVT improves the functional prognosis of LVO stroke even in patients with pre-stroke disability [13]. In an analysis of the HERMES pooled data comparing patients with a pre-stroke mRS score of 0 and patients with a pre-stroke mRS score of 1–2, there was no interaction effect of pre-stroke mRS score on the relationship between the EVT treatment effect and outcome [31]. In patients with pre-stroke disability, FI was achieved less frequently, and RoR was achieved more frequently than in patients without pre-stroke disability. Although patients with pre-stroke disabilities are not expected to achieve functional independence or excellent outcomes after stroke, their ability to return to baseline (RoR) can be a meaningful outcome for their quality of life. Hence, EVT for LVO stroke in patients with pre-stroke disability should not be dismissed. Future trials should consider including patients with pre-stroke disability, considering the endpoints of RoR, and allowing for the generalizability of trial findings to clinical guidelines [9,32].
Mortality was significantly higher in patients with pre-stroke disability than that in patients without pre-stroke disability, similar to previous reports [13-17]. This may be partly related to the significantly increased rates of vascular comorbidities in the prestroke disability group. An observational study reported a higher risk of urinary tract infection and pneumonia within 7 days of admission, a higher risk of malnutrition at discharge, or a greater need for palliative care in acute stroke patients with an mRS score of 3–5 prior to stroke onset compared to those with a pre-stroke mRS score of 0 [33]. There may have been between-group differences in complication rates and post-stroke care plans, but the present study did not collect any related information on these variables. The prevalence of sICH was 6.3% in both groups. Compared to patients without pre-stroke disability, the risks of reperfusion injury or vessel damage by endovascular procedures appear similar in patients with pre-stroke disability. Previous studies have consistently found no significant increase in intracranial hemorrhage after EVT in patients with pre-stroke disability [13-17].
In the present study, the proportion of patients with pre-stroke disability who had an improved mRS score at 90 days compared with the mRS score before the index stroke was 9.9%. The outcome data after EVT for early ischemic stroke in the MR CLEAN registry showed that the proportion of patients with a 90-day mRS score lower than the pre-stroke mRS score was approximately 5% of patients with a pre-stroke mRS score of 2–4 [13]. This seemingly contradictory finding was also reported in other studies [15,16]. Although information on the causes of pre-stroke disability was not collected in this study, including a previous history of stroke, it is conceivable that the 90-day mRS score could be better than the pre-stroke mRS score if transient or recoverable diseases (e.g., infection, bone fracture, or cardiovascular disease) were the cause. In a similar analysis of EVT for early stroke, cardiopulmonary disease and previous stroke were the most frequent causes of disability, followed by musculoskeletal disorder and cognitive impairment [13]. It is quite possible that the cause of pre-stroke disability influences functional prognosis after EVT [34]. In a subgroup excluding patients with mRS score improvement at 90 days, fewer patients with pre-stroke disability achieved FI or RoR than those without. Adding an axis of observation, such as whether the disability is fixed or recoverable, may contribute to a more sophisticated patient selection.
The present study was not intended to compare the societal value of treating acutely ill patients with stroke and pre-stroke disability with that of treating younger, healthier patients without such disabilities. The comparison between the groups was meant to assess whether these patients, excluded if not neglected in current guidelines, could benefit equally, if not similarly, from EVT. In addition, the ASPECTS of the analyzed patients were ≥5, which precludes the application of the present results to large ischemic region stroke [27].
This study has several limitations. First, we analyzed only patients who underwent EVT; hence we concede there is selection bias. Patients selected to undergo EVT by the treating physicians might have been selected based on specific characteristics that were not addressed in this study. In this study, patients with prestroke disability had a lower transfer rate than those without pre-stroke disability, which may suggest a disparity in offering EVT to patients with pre-stroke disability who present to primary stroke centers. Second, the measurement of pre-stroke mRS scores and outcomes was not adjudicated by an independent investigator because of the retrospective nature of this study. While the misjudgment rate of pre-stroke mRS score has been reported to be relatively high [35], it has also been reported that pre-stroke mRS measurements show moderate interobserver agreement [36]. Further information on the arc of the patient’s clinical recovery and quality of life after stroke may be obtained using detailed assessment systems, such as the Barthel Index or Stroke-Specific Quality of Life Measure [37,38]. Third, the analyzed dataset did not include information on cognitive outcomes or pre-stroke cognitive states.
Conclusions
A substantial proportion of patients with late-presenting LVO with pre-stroke disability regained their pre-stroke mRS scores after EVT. Therefore, these patients seem to gain a benefit from treatment similar to patients without pre-stroke disability. EVT may be appropriate for patients with pre-stroke disabilities presenting in the extended time window.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2023.04259.
Univariable, multivariable logistic regression, and IPTW evaluation of FI or RoR at 90 days by pre-stroke mRS: sensitivity analyses
Univariable and IPTW evaluation of outcomes by pre-stroke mRS: excluding pre-stroke mRS of 2
Univariable, multivariable logistic regression, and IPTW evaluation of outcomes by pre-stroke mRS: analysis on imputed data
Distribution of modified Rankin Scale (mRS) at 90 days according to the pre-stroke mRS.
Notes
Funding statement
This study was supported by the Society of Vascular and Interventional Neurology, Japan Agency for Medical Research and Development, Japanese Society for Neuroendovascular Therapy, Ministry of Health, Labor, and Welfare of Japan, Takeda Science Foundation, and Medtronic.
Conflicts of interest
H. Yamagami received research grants from Bristol-Myers Squibb; lecturer fees from Stryker, Medtronic, Johnson & Johnson, Bayer, Daiichi Sankyo, Bristol-Myers Squibb, and Otuska Pharmaceutical; and is an advisory board for Daiichi Sankyo. Siegler reported consultancy fees from Ceribell and involvement in the AstraZeneca Speakers Bureau. Nogueira reported consultancy fees from Biogen, Brainomix, Corindus, Cerenovus, Stryker, Medtronic, Ceretrieve, Anaconda, Biomed, Vesalio, Imperative Care, NeuroVasc Technologies, Viz AI, Genentech, Prolong Pharmaceuticals, Perfuze, Phenox, RapidPulse, and stock options in Viz AI, Vesalio, Perfuze, Corindus, Brainomix, and Ceretrieve, grants from Cerenovus and Stryker. S. Yoshimura reported research grants from Stryker, Siemens Healthineers, Bristol-Myers Squibb, Sanofi, Eisai, Daiichi Sankyo, Teijin Pharma, Chugai Pharmaceutical, HEALIOS, Asahi Kasei Medical, Kowa, CSL Behring and lecturer fees from Stryker, Medtronic, Johnson & Johnson, Kaneka, Terumo, Biomedical Solutions, Boehringer-Ingelheim, Daiichi Sankyo, Bayer and Bristol-Meyers Squibb. N. Sakai received a research grant from Biomedical Solutions, Medtronic, Terumo, and TG Medical; lecturer fees from Asahi-Intec, Biomedical Solutions, Daiichi-Sankyo, Kaneka, Medtronic, and Terumo; and is a member of the advisory boards for Johnson & Johnson, Medtronic, and Terumo. S. Nagel reported consultancy fees from Brainomix and is a speaker with Boehringer Ingelheim and Pfizer. V. Puetz reported lecturer fees from Daiichi Sankyo. Haussen reported consultancy fees from Vesalio, Cerenovus, Stryker, Brainomix, Poseydon Medical, and Chiesi, USA; DSMB from the Jacobs Institute; and stock options in Viz AI. J. P. Marto reported consultancy feed from Amicus Therapeutics and Boehringer Ingelheim and is a Speaker with Boehringer Ingelheim. Sheth reported consultancy fees from Imperative Care, Viz AI, Penumbra, compensation from Motif Neurosciences, and grants from the National Institutes of Health. J. Kaesmacher reported grants from the Swiss Academy of Medical Sciences/Bangerter Foundation, Swiss Stroke Society, and Clinical Trials Unit Bern. D. P. O. Kaiser reported grants from the Joachim Herz Foundation. M. A. Möhlenbruch reported grants from Medtronic, Stryker, and MicroVention. P. A. Ringleb reported travel support from Bayer and Bristol Myers Squibb, and a consultancy for Daiichi Sankyo Company, and Boehringer Ingelheim. M. Ribo reported consultancy fees from Medtronic, MiniMed, Cerenovus, AptaTargets, Stryker, Philips and stock holdings in Methinks, Nora, and Anaconda Biomed. P. Michel reported grants from the University of Lausanne and Swiss National Science Foundation (SNF). T. N. Nguyen disclosed research support from Medtronic to her institution; is a member of the advisory board for Idorsia, Brainomix; and is an Associate Editor of Stroke.
Author contribution
Conceptualization: KT, HY, KU, JES, RGN, SY, NS, TNN. Study design: TKT, HY, KU, JES, RGN, SY, NS, TNN. Methodology: KT, HY, MMQ, JES, RGN, TNN. Data collection: all authors. Investigation: KT, TNN. Statistical analysis: MMQ. Writing—original draft: KT. Writing—review & editing: MMQ, TNN. Funding acquisition: KT, SY, TNN. Approval of final manuscript: all authors.
Acknowledgements
The authors thank Oscar Bolanos of Medtronic.