 |
 |
- Search
| J Stroke > Volume 23(3); 2021 > Article |
|
Abstract
Background and Purpose
In real-world practice, the benefit of mechanical thrombectomy (MT) is uncertain in stroke patients with very favorable or poor prognostic profiles at baseline. We studied the effectiveness of MT versus medical treatment stratifying by different baseline prognostic factors.
Methods
Retrospective analysis of 2,588 patients with an ischemic stroke due to large vessel occlusion nested in the population-based registry of stroke code activations in Catalonia from January 2017 to June 2019. The effect of MT on good functional outcome (modified Rankin Score ≤2) and survival at 3 months was studied using inverse probability of treatment weighting (IPTW) analysis in three pre-defined baseline prognostic groups: poor (if pre-stroke disability, age >85 years, National Institutes of Health Stroke Scale [NIHSS] >25, time from onset >6 hours, Alberta Stroke Program Early CT Score <6, proximal vertebrobasilar occlusion, supratherapeutic international normalized ratio >3), good (if NIHSS <6 or distal occlusion, in the absence of poor prognostic factors), or reference (not meeting other groups’ criteria).
Results
Patients receiving MT (n=1,996, 77%) were younger, had less pre-stroke disability, and received systemic thrombolysis less frequently. These differences were balanced after the IPTW stratified by prognosis. MT was associated with good functional outcome in the reference (odds ratio [OR], 2.9; 95% confidence interval [CI], 2.0 to 4.4), and especially in the poor baseline prognostic stratum (OR, 3.9; 95% CI, 2.6 to 5.9), but not in the good prognostic stratum. MT was associated with survival only in the poor prognostic stratum (OR, 2.6; 95% CI, 2.0 to 3.3).
After several randomized controlled trials (RCTs) failed to demonstrate the superiority of endovascular treatment of stroke over medical management [1,2], the inclusion criteria of the next RCTs were narrowed, excluding patients with better natural history or poor prognostic factors at baseline, that could hamper the identification of the therapeutic effect of vessel revascularization. These RCTs demonstrated the efficacy of mechanical thrombectomy (MT) in patients with stroke due to large vessel occlusion in the anterior circulation [3]. However, in clinical practice, a substantial proportion of patients do not fulfill these inclusion criteria [4]. The Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo (DAWN) trial and Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke 3 (DEFUSE-3) (DAWN NCT02142283; DEFUSE-3 NCT02586415) RCTs extended the evidence for MT to the late time window using advanced imaging [5,6], but evidence for MT’s utility in other patient subgroups or without advanced imaging selection is lacking. Non-randomized reports [7-9] and subgroup analysis of RCTs [10] suggest that the benefit of revascularization may be broader. Here, we estimated the efficacy of MT in patients with a vascular occlusion within a population-based registry of stroke codes characterized by a broader clinical spectrum than patients enrolled in RCTs. Since this is a non-randomized study, we used an inverse probability of treatment weighting (IPTW) analysis from a propensity score (PS) in order to obtain a well-balanced pseudo-population for baseline factors.
This observational study, conducted in accordance with STROBE guidelines (Supplementary Table 1), is based on the Codi Ictus Catalunya (CICAT) registry, a government-mandated, prospective, hospital-based dataset that includes all stroke code activations in Catalonia. We used data from consecutive patients in whom the stroke code was activated directly by the emergency medical services from January 2017 to June 2019. The following variables were registered: demographic information, vascular risk factors, pre-stroke functional status (modified Rankin Scale [mRS]), National Institutes of Health Stroke Scale (NIHSS) at admission, the presence of large vessel occlusion on admission, site of occlusion (proximal occlusion was defined as an intracranial occlusion of the internal carotid, M1 portion of the middle cerebral artery, tandem occlusion, or basilar artery occlusion; distal occlusion was defined as an occlusion distal to M1 portion of the middle cerebral artery, or in the anterior or posterior cerebral artery), revascularization treatment (none, systemic thrombolysis alone, MT with or without thrombolysis), and time metrics including time from onset to imaging and time to revascularization treatment (systemic thrombolysis and MT).
The impact of MT was studied in three pre-defined baseline prognostic groups defined around some of the main inclusion criteria of the pivotal RCTs that demonstrated the efficacy of MT in stroke, selected primarily for being well-established prognostic factors in stroke (not necessarily for potential interactions with the effect of MT). Patients meeting these criteria were classified as the reference prognostic group (premorbid mRS ≤1, age ≤85 years, NIHSS ≤24 and ≥6, time from onset ≤6 hours, Alberta Stroke Program Early CT Score [ASPECTS] ≥6 [11], proximal vascular occlusion in the anterior territory); patients not meeting at least one of the standard inclusion criteria were classified into poor (premorbid mRS >1, age >85 years, NIHSS ≥25, time from onset >6 hours, large infarct with ASPECTS <6, proximal occlusion in the vertebrobasilar territory, supratherapeutic international normalized ratio >3), and good (if NIHSS <6 or distal occlusion in the anterior or posterior territory in the absence of any of the poor-prognosis features) prognostic groups. The primary outcome measures were centrally evaluated 3 months after the stroke and included functional outcome and vital status (good functional outcome defined as mRS ≤2, survival as mRS <6). The univariate distribution of the primary outcome measures was reported in each prognostic group according to the treatment received. Symptomatic intracranial hemorrhage was defined according to the European Cooperative Acute Stroke Study II (ECASS II) criteria [12]. Successful recanalization following MT was defined as a grade 2b or 3 according to the modified thrombolysis in cerebral ischemia scale [13]. The ASPECTS score was not a mandatory variable in our registry but may have influenced treatment choice and was used for the study group assignment. For this reason, a sensitivity analysis for the primary outcomes was conducted after multiple data imputations for missing values, including ASPECTS.
This is a Real-World Evidence (RWE) analysis using the population-based CICAT registry, which satisfies all legal requirements mandated by the local law of personal data protection. The dataset was processed and analyzed according to local and European laws: Regulation (EU) 2016/679 of the European Parliament and of the Council of April 27, 2016, on Data Protection and Spanish Organic Law 3/2018, of December 5, on Protection of Personal Data and guarantee of digital rights. The Ethical Committee at Hospital Clínic approved the study (registry code HCB/2019/0716). Informed consent was waived because of the retrospective nature of the study.
Continuous variables were described as mean±standard deviation or median with interquartile range (IQR), as appropriate. Categorical variables as absolute frequencies and percentages, or median with IQR for ordinal categorical variables. We used standardized differences, defined as differences between groups divided by pooled standard deviation, to assess heterogeneity between cohorts for baseline covariables.
To assess the impact of an intervention on the primary outcomes in the absence of randomization, we used an IPTW analysis on PS suitable for multiple confounders in observational studies. The purpose of IPTW analysis is the creation of pseudopopulations with low associations between treatment, confounders and indication bias. This methodological approach produces groups in which the treatment assignment is independent of measured baseline covariates by weighting subjects by the inverse probability of treatment received [14,15]. The estimation of the IPTW was performed calculating the PS from a logistic regression model to receive MT according to the variables described in Table 1 and stabilized by the proportion of MT or medical treatment. IPTW-weighted logistic regression models were used to estimate the odds ratio (OR) and their 95% confidence interval (CI) of good functional outcome and survival at 3 months. These analyses were made for each prognosis stratum and included age, pre-stroke mRS, systemic thrombolysis, NIHSS score, and occlusion site. We checked for the adequate balance of baseline covariates after IPTW analyses in each prognostic stratum by calculating standardized differences, and a difference greater than ±0.20 represented a meaningful imbalance [16]. In this analysis, the maximum standardized difference was 0.145, corresponding to baseline mRS for poor prognosis.
The primary analysis did not include the ASPECT scale in IPTW calculation due to a high proportion of missing data (1,324 patients, 1,016 [49%] treated with MT, and 308 [48%] with medical management alone). A sensitivity analysis was made, including the ASPECTS scale with missing data imputation to the previously described logistic regression model. We used the expectation-maximization algorithm [17], which relies on the flexible and reasonable missing at random assumption using age, sex, delay to radiological evaluation, NIHSS, mRS, comorbidities as hypertension, diabetes, dyslipidemia, atrial fibrillation, coronary heart disease, presence of a previous stroke, actual smoke, and presence of distal occlusion.
We calculated the number needed to treat (NNT) for saving a patient from poor outcomes. NTT was estimated according to logistic regression models used in the primary analysis adapting the calculation proposed by Bender and Blettner [18] and Bender et al. [19] to present context by means:
Where OR was estimated from IPTW-weighted logistic regression models and P0 was the proportion of non-event.
In all statistical analyses, we applied a two-sided type I error of 5%. SPSS version 25 (IBM Co., Armonk, NY, USA) and SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) were used for the analysis.
From 15,774 stroke code activations during the study period, 10,117 had an ischemic stroke, and 3,989 had a vessel occlusion identified on initial imaging. After excluding patients with missing information, the analysis included 2,588 patients (Figure 1). Patients excluded from the analysis were younger and received systemic thrombolysis in a lower proportion than those included, but the other variables showed similar distribution according to the standard difference values (Supplementary Table 2).
In the whole study cohort, 1,996 patients received MT and 592 medical management alone. Successful recanalization was achieved in 83% of patients treated with MT. Patients receiving MT were more likely to belong to the reference and poor category groups, were younger, had less pre-stroke disability, received systemic thrombolysis less frequently, and had better ASPECTS scores (Table 1). The pre-defined prognostic groups according to baseline characteristics included 976 patients (38%) in the reference group, 1,191 patients (46%) in the poor prognosis group, and 421 patients (16%) in the good prognosis group. The description of the prognostic factors determining group assignment is detailed in Supplementary Table 3.
The functional status at 3 months in the study cohort according to the treatment received in each prognostic group without IPTW adjustment are summarized in Figure 2. Any hemorrhage in follow-up imaging was more frequently found in patients treated with MT compared to those treated with only medical treatment in all prognosis subgroups (Table 2).
The standard differences of the clinical and radiological variables at baseline between patients who received MT and those who received medical treatment alone were adequately balanced after IPTW in the whole cohort (Figure 3) and stratified by prognostic groups (Supplementary Table 4). In the IPTW logistic regression model, MT was related to good outcomes in the subgroups of reference (OR, 2.94; 95% CI, 1.96 to 4.35; P<0.0001) and poor prognosis (OR, 3.85; 95% CI, 2.56 to 5.88; P<0.0001), but not in the good prognostic category (OR, 1.23; 95% CI, 0.85 to 1.79; P=0.27). MT was associated with survival only in the poor prognosis category (OR, 2.56; 95% CI, 1.96 to 3.33; P<0.001), more details are shown in Table 3 and Figure 4. Consequently, the NNT for good outcome was 4 (95% CI, 3 to 7) in the reference prognosis group, 4 (95% CI, 2 to 5) in the poor prognosis group, and not interpretable because the CI does not include the NNT value in the good prognosis group (21; 95% CI, -41 to ∞ to 7).
The sensitivity analyses after multiple data imputations confirmed the associations between MT and functional outcome. MT remained associated with good outcomes in the reference and poor baseline prognosis category groups. MT was associated with survival in the whole cohort of the sensitive analysis but did not reach signification when assessed for each prognostic category (Table 3 and Figure 4).
This sizeable and representative population-based registry confirmed the benefit from MT in terms of functional outcome and survival in real-life practice, mainly in patients with non-favorable prognostic factors at baseline. Consequently, it also suggested that the effect of MT was not homogenous in all patients with stroke and vessel occlusion, raising doubts on the efficacy of current revascularization techniques in patients with specific characteristics such as mild symptoms or distal occlusions. In contrast, patients with the poorest prognostic factors benefit substantially from MT.
The concerns about the external validity of the results generated in large RCTs addressing the efficacy of MT in large vessels occlusions are emphasized by the finding that in this multi-center registry reflecting clinical practice in Catalonia, more than half of the patients treated with MT did not meet the main inclusion/exclusion criteria used in most of the studies that confirmed the efficacy of MT versus best medical treatment. These results are reassuring when dealing with such patients and raise the question of whether the efficacy of MT in certain subgroups of patients may be best tested in studies like this, rather than in randomized clinical trials that are sometimes unpractical and whose results may not be generalized to all patients.
Although the severity of the symptoms did not significantly modify MT’s effect in subgroup analyses of the thrombectomy RCTs [3], as usual in most designs of RCTs, included patients are relatively homogeneous, which induces a selection bias. In the end, the vast majority of patients in those trials had moderate to severe strokes. Our registry has good internal validity and confirms the findings of observational reports describing decreased MT benefits in patients with milder strokes [20-22]. Overall, the evidence suggests that the risk of futile endovascular intervention is highest in patients with low NIHSS at baseline or distal occlusions. It is expected that the results of the ongoing Minor Stroke Therapy Evaluation RCT (NCT03796468) will shed light on the efficacy of MT in patients with mild strokes.
Inversely, patients included in the poor baseline prognostic stratum benefited as much as patients in the reference prognostic stratum. This is in line with recent observations describing few complications and potential benefits of thrombectomy in groups of patients with large infarctions [7,10], or other poor prognostic factors such as poor collateral circulation [8] and older age [23]. At the same time, these results support the use of broad inclusion criteria in RCTs testing MT in stroke, as excluding patients with certain poor prognostic factors may paradoxically reduce the treatment’s effect size [24]. Nevertheless, the overall clinical outcome is still poor in about two out of three patients of this subgroup of patients, meaning that they may benefit from better revascularization techniques, additional neuroprotectant strategies, or even improved imaging selection to identify extensive irreversible damage better. Although perfusion imaging is commonly used to select patients in the late time window in our population, technical parameters and operative criteria differed between centers, and quantitative data were not available in the registry.
The study has some limitations, primarily linked to its observational design, mainly the obvious prescription bias we tried to overcome with the IPTW statistical analysis technique. However, observational studies performed in large multicenter cohorts are vital to confirm the real-life clinical impact of the effect of interventions proved to be beneficial in clinical trials. The assessment of the baseline ischemic lesion using ASPECTS was optional in the registry and was available only in half of the patients, not allowing us to include it in the calculation of the IPTW. However, in the sensitivity analysis using missing imputation for patients without the ASPECTS value, the effect of MT on functional outcome and survival was similar to that of the main analysis, despite a reduced effect in the poor prognostic stratum (non-significant trend for survival), which reflects the prognostic value of ASPECTS. The evidence in favor of thrombectomy has gradually changed over time, and it could be argued that the definition of the groups in the study could be done differently. However, the objective of this analysis was not to study the effect of each specific prognostic factor, but to compare the impact of MT across different prognostic groups in a way that tries to minimize the influence of confounding factors. This is the main strength of the primary results of the study, stressing that the impact of MT is greater in patients with poorer overall prognosis.
This RWE analysis of a population-based registry reassures physicians considering MT for patients with poor prognostic indicators at baseline. Conversely, it suggests that extending the utility of MT to specific subgroups of patients with better natural history may require further research and technical advances.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2021.00962.
Supplementary Table 1
STROBE statement—Checklist of items that should be included in reports of cohort studies
Supplementary Table 2.
Baseline characteristics of the cohort included and excluded for the presence of missing data (except for ASPECTS) in the final analysis
Supplementary Table 3.
Characterization of the factors determining the assignment of patients to poor or good prognosis categories
Supplementary Table 4.
Standardized differences after IPTW in the whole cohort and in the pre-specified prognostic strata
Notes
Catalan Stroke Code and Reperfusion (Cat-SCR) Consortium
Bellvitge, Hospitalet de Llobregat (Pere Cardona; Helena Quesada; Blanca Lara; Andrés Paipa; Ana Nuñez Guillen; Roger Barranco; Lucia Aja; Paloma Mora; Oscar Chirife; Sonia Aixut; Maria Angeles de Miquel; Toni Martínez-Yelamos). Vall d’Hebron, Barcelona (Carlos Molina; Marta Rubiera; Jorge Pagola; David Rodríguez-Luna; Sandra Boned; Marian Muchada; Alejandro Tomasello; Marc Ribó; Carlos Piñana; Manuel Requena; Matías Deck; Alvaro Garcia-Tornel; Marta Olivé; Noelia Rodriguez; Jesus Juega). Clínic, Barcelona (Ángel Chamorro; Sergio Amaro; Xabier Urra; Laura Llull; Arturo Renú; Salvatore Rudiloso; Juan M. Macho; Jordi Blasco; Luis San Roman Manzanera; Antonio López; Federico Zarco; Ramón Torné; Ricard Valero; Víctor Obach, Víctor Vera; Alejandro Rodriguez; Martha Vargas; Carlos Laredo). Germans Trias, Badalona (Mònica Millán; Natalia Pérez de la Ossa; Meritxell Gomis; Laura Dorado; María Hernández-Pérez; Anna Ramos; Alejandro Bustamante; Sebastiá Remollo; Carlos Castaño, Mariano Werner). Sant Pau, Barcelona (Joan Martí-Fàbregas; Raquel Delgado-Mederos; Alejandro Martínez-Domeño; Pol Camps-Renom; Luis Prats-Sánchez; Daniel Guisado-Alonso; Marina Guasch-Jiménez; Rebeca Marín Bueno; Jordi BraneraPujol; José Pablo Martínez, Lavinia Dinia). Joan XXIII, Tarragona (Anna Pellisé; Xavier Ustrell; Alan Flores; Laia Seró). Josep Trueta, Girona (Joaquín Serena; Yolanda Silva; Mikel Terceño; Saima Bashir; Víctor Vera; Alan Murillo). Mútua de Terrassa (Jerzy Krupinski; Sonia Huertas; Jessica Molina; Georgina Figueras; Sarah Besora). Mar, Barcelona (Ana RodríguezCampello; Jaume Roquer; Ángel Ois; Eva Giralt-Steinhauer; Elisa Cuadrado-Godia; Jordi Jiménez-Conde; Elio Vivas; Polo Guimaraens). Taulí, Sabadell (David Cánovas; Maria del Carmen Garcia; Jordi Estela; Joan Perendreu; Nicolas Romero; Roberto Eduardo Correa; Oriol Barrachina). Moisès Broggi, Sant Joan Despií (Manuel Gómez-Choco; Sonia M. García; Maria Àngels Font Padrós; Juan José Mengual Chirife, Luis Mena Romo). Mataró (Ernest Palomeras; Virginia Casado; Nicolau Guanyabens; Marta Álvarez). Camils-Garraf (Esther Catena; José Luis Camacho Velásquez). Arnau de Vilanova, Lleida (Francisco Purroy; Gerard Mauri Capdevila; Cristina Garcia). Alt Penedès-Vilafranca (Esther Catena, Jessica García Alhama; Irene Bragado Trigo). Igualada (Jordi Monedero; Mònica Perecaula, Luis Guillermo Casanovas; Carla Colom). Granollers (Dolores Cocho; Adela Rios González). Verge de la Cinta, Tortosa (Juanjo Baiges; Josep Zaragoza; Sonia Escalante; Patricia Esteve). Vic (Josep Maria Aragonés). Althaia, Manresa (Júlia Saura; Josep Maria Soler-Insa; Natalia Mas). Campdevànol (Glòria Diaz; Margarida Vergés). Figueres (Xavier Costa; Liseth Molina). Palamós (M. Cruz Alemendros; Marc Pérez; Ana Cabanelas; Olga Belchi). Olot (Maria Rybyeba). Cerdanya (Miquel Barceló). Mora Ebre (Dolors Carrión). Seu Urgell (Carmen Repullo). Tremp (Eduard Sanjurjo). Oficina Seguiment (avaluació clínica 3m) (Mercè Salvat-Plana; Josep Roig; Verònica Hidalgo; Olga Fagúndez; Victòria Sala). SEM (Anabel Alonso; Marisol Querol; Montse Gorchs; Xavier Jiménez; Maria Àngels Mora).
Acknowledgments
We thank Martha Vargas and Guillem Gallofre for handling the databases for this study. This work was supported by grants from Fondo de Investigacions Sanitarias of the Institut de Salud Carlos III to Ángel Chamorro and Xabier Urra (FIS-ISCIII PI18/00444) co-financed by the Fondo Europeo de Desarrollo Regional (FEDER). Xabier Urra is sponsored by the Instituto de Salud Carlos III, reference number INT19/00020, and by the European Social Fund (The ESF-Investing in your future). Salvatore Rudilosso receives funding from the Institute of Health Carlos III, with a Grant for Health Research (CM18/00116).
Figure 1.
Study selection process. The flow-diagram shows the patients included in the analysis. TIA, transient ischemic attack; SAH, subarachnoid hemorrhage. *Missing values were vascular risk factors (hypertension, diabetes mellitus, dyslipidemia, atrial fibrillation, coronary heart disease, previous stroke/TIA, smoking habit variables) in 401 patients, delay to imaging in 214, and occlusion site in 503.

Figure 2.
Primary outcome measures without inverse probability of treatment weighting adjustment. The Sankey diagram showing the treatment and outcomes in each baseline prognostic category. MT, mechanical thrombectomy; mRS, modified Rankin Scale.
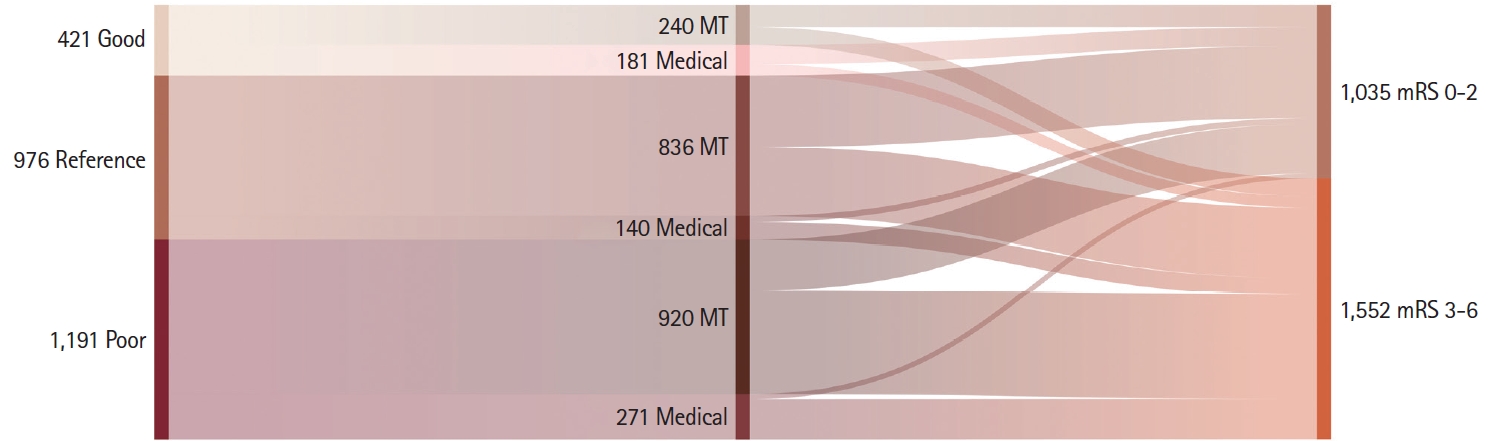
Figure 3.
Standardized differences before and after inverse probability of treatment weighting (IPTW). Standardized differences between mechanical thrombectomy and medical treatment before and after IPTW. mRS, modified Rankin Scale; TIA, transient ischemic attack; NIHSS, National Institutes of Health Stroke Scale.
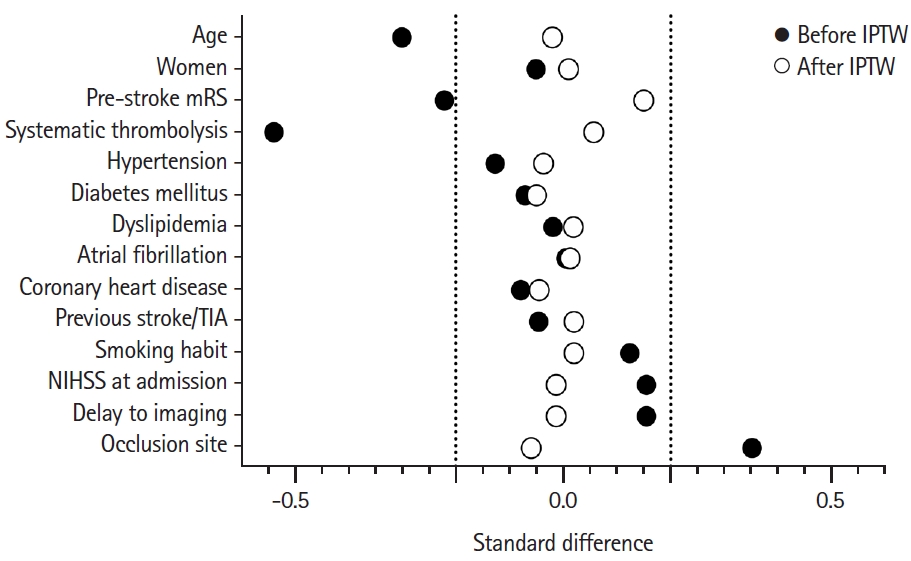
Figure 4.
Primary outcome analysis. The forest plots illustrate the treatment effect in each group in terms of good functional outcome and survival in the main analysis (A) and in the sensitive analysis (B) after inverse probability of treatment weighting (IPTW) analysis. The sensitive IPTW analysis included the Alberta Stroke Program Early CT Score (ASPECTS) variable in the IPTW calculation after missing data imputation. OR, odds ratio; CI, confidence interval; MT, mechanical thrombectomy.

Table 1.
Baseline characteristics of the treatment groups
Values are presented as mean±standard deviation, number (%), or median (interquartile range). Standard difference was considered acceptable if not greater than ±0.20.
mRS, modified Rankin Scale; TIA, transient ischemic attack; NIHSS, National Institutes of Health Stroke Scale; ASPECTS, Alberta Stroke Program Early CT Score; M2, second segment of the middle cerebral artery; ACA, anterior cerebral artery; PCA, posterior cerebral artery; M1, first segment of the middle cerebral artery; TICA, terminal internal carotid artery; VB, vertebro-basilar.
Table 2.
Clinical course, radiological outcomes, and safety outcome measures
Values are presented as number (%) or median (interquartile range).
MT, mechanical thrombectomy; TICI, thrombolysis in cerebral ischemia; HI1, hemorrhagic infarction type 1 (small petechiae along the margins of the infarct); HI2, hemorrhagic infarction type 2 (confluent petechiae within the infarcted area but no space-occupying effect); PH1, parenchymal hematoma (blood clots in ≤30% of the infarcted area with some slight space-occupying effect); PH2, parenchymal hematoma (blood clots in >30% of the infarcted area with a substantial space-occupying effect); rPH, remote parenchymal hematoma; NIHSS, National Institutes of Health Stroke Scale.
Table 3.
Main and sensitivity analysis for outcome by logistic regression models with IPTW
References
1. Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 2013;368:893-903.



2. Chimowitz MI. Endovascular treatment for acute ischemic stroke—still unproven. N Engl J Med 2013;368:952-955.


3. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after largevessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723-1731.


4. Urra X, Abilleira S, Dorado L, Ribó M, Cardona P, Millán M, et al. Mechanical thrombectomy in and outside the REVASCAT trial: insights from a concurrent population-based stroke registry. Stroke 2015;46:3437-3442.


5. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018;378:11-21.


6. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, OrtegaGutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018;378:708-718.



7. Sarraj A, Hassan AE, Savitz S, Sitton C, Grotta J, Chen P, et al. Outcomes of endovascular thrombectomy vs medical management alone in patients with large ischemic cores: a secondary analysis of the optimizing patient's selection for endovascular treatment in acute ischemic stroke (SELECT) study. JAMA Neurol 2019;76:1147-1156.



8. Renú A, Laredo C, Montejo C, Zhao Y, Rudilosso S, Macias N, et al. Greater infarct growth limiting effect of mechanical thrombectomy in stroke patients with poor collaterals. J Neurointerv Surg 2019;11:989-993.


9. Renú Jornet A, Urra X, Laredo C, Montejo C, Rudilosso S, Llull L, et al. Benefit from mechanical thrombectomy in acute ischemic stroke with fast and slow progression. J Neurointerv Surg 2020;12:132-135.


10. Román LS, Menon BK, Blasco J, Hernández-Pérez M, Dávalos A, Majoie CBLM, et al. Imaging features and safety and efficacy of endovascular stroke treatment: a meta-analysis of individual patient-level data. Lancet Neurol 2018;17:895-904.

11. Kaesmacher J, Chaloulos-Iakovidis P, Panos L, Mordasini P, Michel P, Hajdu SD, et al. Mechanical thrombectomy in ischemic stroke patients with alberta stroke program early computed tomography score 0-5. Stroke 2019;50:880-888.



12. Hacke W, Kaste M, Fieschi C, von Kummer R, Davalos A, Meier D, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet 1998;352:1245-1251.


13. Khatri P, Hill MD, Palesch YY, Spilker J, Jauch EC, Carrozzella JA, et al. Methodology of the interventional management of stroke III trial. Int J Stroke 2008;3:130-137.



14. Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 2015;34:3661-3679.



15. Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput 2009;38:1228-1234.

16. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 2009;28:3083-3107.



17. Dempster AP, Laird NM, Rubin DB. Maximum likelihood from incomplete data via the EM algorithm. J R Stat Soc Series B Methodol 1977;39:1-22.


18. Bender R, Blettner M. Calculating the "number needed to be exposed" with adjustment for confounding variables in epidemiological studies. J Clin Epidemiol 2002;55:525-530.


19. Bender R, Kuss O, Hildebrandt M, Gehrmann U. Estimating adjusted NNT measures in logistic regression analysis. Stat Med 2007;26:5586-5595.


20. Sarraj A, Hassan A, Savitz SI, Grotta JC, Cai C, Parsha KN, et al. Endovascular thrombectomy for mild strokes: how low should we go? Stroke 2018;49:2398-2405.



21. Urra X, San Román L, Gil F, Millán M, Cánovas D, Roquer J, et al. Medical and endovascular treatment of patients with large vessel occlusion presenting with mild symptoms: an observational multicenter study. Cerebrovasc Dis 2014;38:418-424.


22. Goyal N, Tsivgoulis G, Malhotra K, Ishfaq MF, Pandhi A, Frohler MT, et al. Medical management vs mechanical thrombectomy for mild strokes: an international multicenter study and systematic review and meta-analysis. JAMA Neurol 2020;77:16-24.










