National Trends in Clinical Outcomes of Endovascular Therapy for Ischemic Stroke in South Korea between 2008 and 2016
Article information
Dear Sir:
The advent of mechanical thrombectomy (MT) in 2015 drastically changed the treatment of acute stroke [1]. The corresponding guidelines were revised in 2019 to broaden the scope of MT within 24 hours of symptom onset [2]. In previous studies, MT have improved the prognoses of patients in real-world clinical settings [3,4]. Using nationwide representative data, this study aimed to evaluate the national trends in clinical outcomes of patients treated with endovascular therapy (ET) in South Korea.
From the Korean National Health Insurance Service database [5], we extracted the claims data of patients aged >45 years who were hospitalized due to cerebral infarction (International Classification of Diseases, 10th revision, code: I63) and underwent ET (based on the registered procedure codes) between 2007 and 2017. We categorized the analysis period as follows: the “non-advanced MT period (January 2008 to December 2010),” when stent retrievers were rarely used; “transitional period (January 2011 to July 2014),” when stent retrievers were used off-label and were not reimbursed; and the “MT period (August 2014 to December 2016),” when the insurance claims data verified the frequency of stent retriever use. We categorized the status of discharge to home as a good outcome and statuses of cerebral hemorrhage, disability, and death as poor outcomes. SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was used to perform statistical analysis. Methods are provided in detail in the Supplementary methods. This study was approved by the Institutional Review Board of the National Health Insurance Service Ilsan Hospital (NHIMC 2019-01-006).
Between 2008 and 2016, a total of 12,501 patients with acute ischemic stroke were treated with ET. In 2015, ET was administered at a higher rate than that in the previous year. During the study period, the annual rate of discharge to home significantly increased, whereas the rates of cerebral hemorrhage, disability, and death significantly decreased (P<0.0001) (Figure 1). The rate of home discharge was 35.8% in 2008 and 43.8% in 2016. The 3-month mortality rate was 27.2% in 2008 and 19.7% in 2016. The ratio of patients receiving surgery for cerebral hemorrhage within 30 days gradually decreased from 6.8% in 2008 to 1.8% in 2016. Furthermore, the rate of disability was 36.8% in 2008 and 21.7% in 2016.
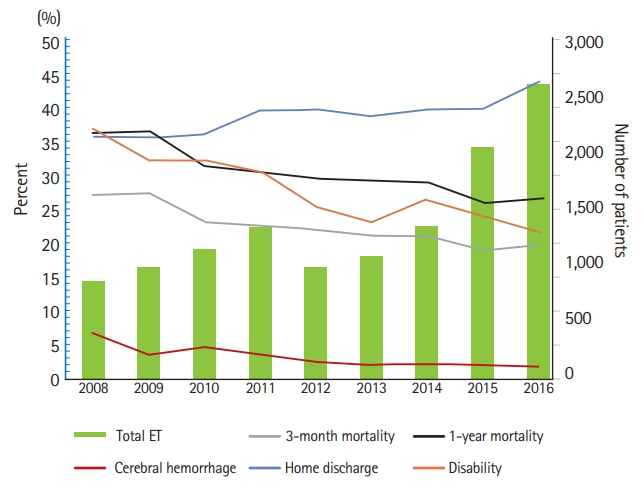
Annual trends among patients treated for ischemic stroke with endovascular therapy (ET) from 2008 to 2016 and their outcomes. All P-values were <0.0001 on the Cochran-Armitage trend test.
A period-based analysis revealed that the patients’ average age and the prevalence of risk factors increased gradually during the study period. The highest proportion of comorbidities and Charlson comorbidity index was noted in the MT period. The rate of home discharge increased and the mortality rates decreased continuously from the non-advanced MT period to the MT period. Additionally, the ratio of the patients receiving surgery for cerebral hemorrhage after ET decreased during the study period. The rate of disability after ischemic stroke also showed a significant decrease from the non-advanced MT period to the MT period (Table 1). The 1-year survival rate tended to increase from the non-advanced MT period to the MT period (P<0.0001) (Figure 2). After adjusting for age, sex, comorbidities, and use of tissue plasminogen activator, the risk of death and disability were significantly lower in the MT and transitional periods than in the non-advanced MT period. Logistic regression analysis adjusted for the same covariates revealed the MT period was an independent predictor of home discharge (Supplementary Table 1).

Baseline characteristics and outcomes of patients according to the period of endovascular therapy adoption
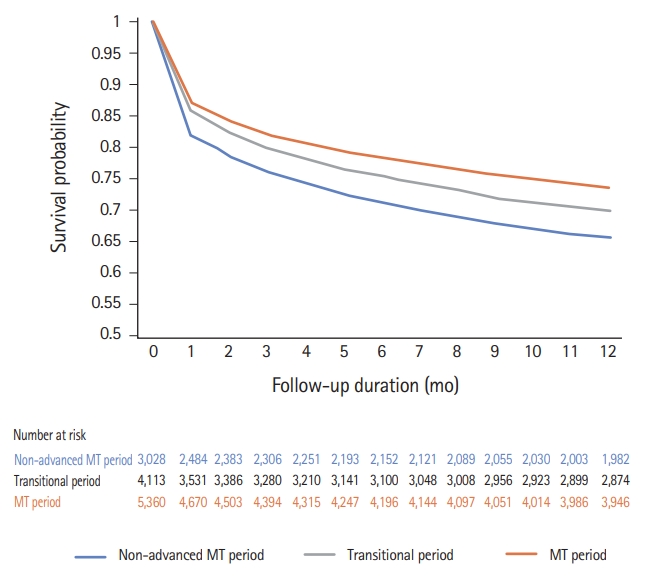
Kaplan-Meier curve of 1-year mortality in the patients treated for ischemic stroke by the period of endovascular therapy adoption (P<0.0001). MT, mechanical thrombectomy
In agreement with other studies [3,4], our analysis of the nationwide data showed that the patients treated with ET had better outcomes in the MT period than in the non-advanced MT period. Over time, the baseline prognostic characteristics, reflected by age and comorbidities, got worse; however, the outcomes of the patients generally improved; this was supported by the annual trend analyses (Supplementary Table 2).
In this study, the rates of mortality, disability, and cerebral hemorrhage decreased with the increased application of ET. The 3-month mortality rate in the MT period observed in the current study was higher than that reported in a meta-analysis of pivotal clinical trials [6], but it was lower than that reported in a real-world data study [7]. The 3-month mortality rate during the transitional period was similar to that reported by a study performed around the time when stent retrievers were introduced [8]. We could not verify the clinical data from this claim data; therefore, we used disability registration data following cerebral injury rather than modified Rankin Scale (mRS) to evaluate patient prognosis. The ratio of patients with an mRS of 3–5 (vs. 0–2) at 3-months in the meta-analysis of clinical studies and real-world data was higher than the rate of patients with cerebral injury-related disability among the patients in the national database used in our study [6,7]. This difference could possibly because some patients with an mRS of 3–5 at 3 months would have returned to their daily lives after rehabilitation. When patients survive with a disability after a stroke event, their direct medical costs and indirect social costs increase [9]. Therefore, verifying decreases in the number of such disabled patients is meaningful.
This study has several limitations. We used insurance claims data rather than well-designed clinical trial or prospective registry data. Therefore, we were unable to adjust for detailed and important prognostic factors such initial National Institutes of Health Stroke Scale scores, occlusion sites, recanalization status, and interval from symptom onset to recanalization. In addition, we were unable to verify the precise number of patients who received ET in the period when solitaire stents, the most common ET instrument, were only used off-label or when the solitaire stents were not covered by insurance. Improved outcomes of patients treated with ET in the transitional period compared to those of patients treated with ET in the non-advanced MT period is likely attributed to the increasing use of MT. However, we had no data on the proportion of patients treated with MT during the transition period and our interpretation is not supported by formal analysis.
In conclusion, our analysis of nationwide insurance data verified that the rates of mortality and disability associated with stroke have decreased with the increasingly widespread adoption of stent retrievers.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2020.01928.
Univariate analysis of outcome predictors (mRS 0–3)
Baseline characteristics and outcomes of patients according to the calendar year
Acknowledgements
This work was supported by the National Health Insurance Ilsan Hospital grant (2019-1-167). This study used NHIS-NHID data (2019-1-167), provided by National Health Insurance Service (NHIS). The authors alone are responsible for the content and writing of the paper.
Notes
The authors have no financial conflicts of interest.
