 |
 |
- Search
| J Stroke > Volume 21(3); 2019 > Article |
|
Several studies have demonstrated that Mediterranean diet (MeD) has beneficial effects in the prevention of cardiovascular disease (CVD) [1,2] globally but also in stroke prevention [3,4]. However, there are few data of the influence of MeD in silent brain infarcts (SBI). Physical activity is also a well-known protective factor for CVD and stroke [5]. Atrial fibrillation (AF) increases the risk of overt stroke and also SBI. We hypothesize that a healthy lifestyle would reduce the rate of SBI among AF patients. The aim of this study is to determine the association of a healthy profile (the combination of a good MeD adherence plus high level of physical activity) and the prevalence of SBI in a population with AF.
To determine this association we have selected patients diagnosed of non-valvular AF (NVAF) from Seville urban area were selected from DIRAYA, the Andalusian electronic healthcare database. The inclusion criteria were: patients diagnosed of NVAF (according to International Classification of Diseases, 9th revision [ICD-9] classification) who scored 0-1 in the CHADS2 score, age Ōēź50 years and patients who give their consent. Patients were excluded when they had history of previous stroke/transient ischemic attack, if brain magnetic resonance imagine (MRI) was contraindicated or claustrophobia or when receiving oral anticoagulation. A total of 915 eligible patients were selected. A phone-call was made to explain the study protocol. After inclusion, patients were scheduled for a brain 3T-MRI. Baseline visit was performed at the same time and demographical data and medical history were collected. Physical activity and diet habits were also assessed by two validated self-administered questionnaires, the International Physical Activity Questionnaire (IPAQ) [6] and the 14-item questionnaire of adherence to MeD from the Prevenci├│n con dieta mediterr├Īnea (PREDIMED) Study [2]. All MRI scans were performed with the same 3.0 Tesla MR (Philips Ingenia CX, Release 3.1, Koninklijke, Amsterdam, the Netherlands). MRI protocol included: sagittal 1 mm 3DT1-weighted gradient echo (GRE), sagittal 1,12 mm 3DT2-weighted fat sat fluid-attenuated inversion recovery (FLAIR), axial 5 mm 2DT2*-weighted GRE, and axial 3 mm 2D diffusion-weighted imaging (DWI [B0, B1000, ADC map]). SBI were defined as focal lesions with roughly the same intensity of cerebrospinal fluid. SBI were classified into acute/subacute lesions (hyperintense signal lesion on DWI) and chronic lesions (hyperintense FLAIR signal lesions with hypointense signal on T1-weigted images). In doubtful cases, we also analyzed the presence of complete surrounding FLAIR hyperintensities as another criterion following the standards for reporting vascular changes in neuroimaging (STRIVE) guidelines [7].
Statistical analysis was performed with the SPSS version 21.0 statistical package (IBM Co., Armonk, NY, USA). Cutoff values for age and alcohol intake were determined using receiver operating characteristic (ROC) analysis. To determine the independent risk factors of SBI, multivariable regression analysis was performed. Results are shown as odds ratio (OR), 95% confidence intervals (CIs), and P-values. The study protocol and consent forms were approved by the Ethics Committee of Virgen del Roc├Ło University Hospital (reference no.2014PI/162-1).
Of 443 patients included from May 2015 to June 2016, 66 patients (14.9%) presented at least 1 SBI on MRI. Baseline characteristics are shown in Supplementary Table 1.
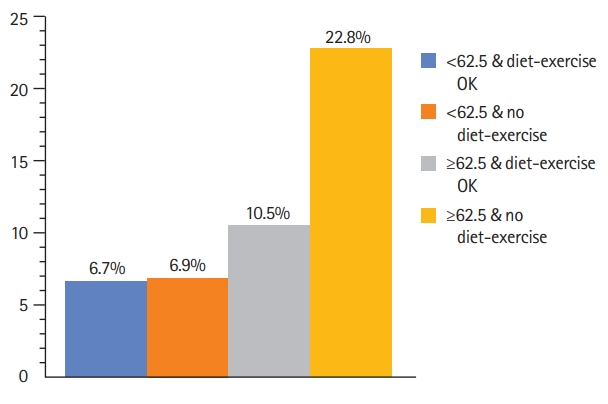
Univariate analysis (Supplementary Table 2) showed that an older age (71 years old vs. 65 years old, P=0.001), and higher alcohol intake, defined by consumption of >78 g/week (36.4% vs. 22.3%, P=0.014) were associated with higher risk of SBI. There was no association of SBI with MeD adherence nor physical activity when considered individually. Patients with a high adherence to MeD were more physically active (40.6% vs. 34.6%, P=0.028) (Supplementary Figure 1). A variable that combines a good adherence to MeD (score 8-14 in the questionnaire) [8] plus high level of physical activity (Ōēź3,000 metabolic equivalents [METS]/week) was created (healthy profile). In univariate analysis healthy profile was associated with a lower risk of SBI (16.6% vs. 30%, P=0.035). After logistic regression analysis adjusted by vascular risk factors (Table 1), age Ōēź62.5 years was an independent predictor of SBI (OR, 3.47; 95% CI, 1.72 to 6.97; P<0.001) and a healthy profile was independently associated with a lower risk of SBI (OR, 0.49; 95% CI, 0.24 to 0.98; P=0.046). Patients Ōēź62.5 years with low adherence to MeD plus low/moderate level of physical activity had high frequency of SBI (22.8%) (Figure 1).
According to our results, a healthy lifestyle defined by a moderate/high adherence to MeD and a high level of physical activity (>3,000 METS/week) might have a protective effect on SBI prevalence in patients with NVAF. This association with MeD has been previously reported [9]. Moreover, MeD adherence has been associated with a reduction of cardiovascular events in patients with AF through an antioxidant effect [10]. Our study was performed in a population with AF, so as they have an increased risk of stroke, prevention should be more intensive regarding lifestyle. When we considered diet and physical activity as independent variables, we have not found any statistically significant association. This may be explained because people who are more adherent to MeD may be more healthy conscious and indeed more physically active (Supplementary Figure 1). Moreover, this population is thought to smoke less or consume less alcohol, but these confounders were also taken into account [11]. Our study is a single center study in Andalusia, Spain, a region in which MeD is the most frequent type of diet, but our results are consistent with other studies conducted in our country [2].
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2019.01949.
Supplementary┬ĀFigure┬Ā1.
Graphic showing distribution of patients regarding adherence to Mediterranean diet and physical activity.
Acknowledgments
The Spanish Ministry of Economy, Industry and Competitiveness (grant RTC-2016 5300-1), the Junta de Andaluc├Ła (grant PIN-0144-2016), the European Project ITRIBIS (registration number REGPOT-2013-1) and Cooperative Cerebrovascular Disease Research Network (INVICTUS+, RD16/0019/0015) supported the study. The Fundaci├│n Cajasol also contributed to the study.
Figure┬Ā1.
Silent brain infarct (SBI) prevalence according to age and ŌĆ£healthy profile.ŌĆØ This figure shows the prevalence of SBI in different groups of patients according to age and the combination of adherence to Mediterranean diet and physical activity.
Table┬Ā1.
Multivariable analysis of silent brain infarct risk factors
References
1. Rosato V, Temple NJ, La Vecchia C, Castellan G, Tavani A, Guercio V. Mediterranean diet and cardiovascular disease: a systematic review and meta-analysis of observational studies. Eur J Nutr 2019;58:173-191.



2. Estruch R, Ros E, Salas-Salvad├│ J, Covas MI, Corella D, Ar├│s F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med 2018;378:e34.


3. Tsivgoulis G, Psaltopoulou T, Wadley VG, Alexandrov AV, Howard G, Unverzagt FW, et al. Adherence to a Mediterranean diet and prediction of incident stroke. Stroke 2015;46:780-785.



4. Psaltopoulou T, Sergentanis TN, Panagiotakos DB, Sergentanis IN, Kosti R, Scarmeas N. Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol 2013;74:580-591.


5. OŌĆÖDonnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet 2016;388:761-775.


6. Craig CL, Marshall AL, Sj├Čstr├Čm M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381-1395.


7. Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 2013;12:822-838.



8. Gonz├Īlez Morales I, Torres Amengual M, Mart├Łnez Fern├Īndez CA, Luque Vara T. The Mediterranean diet in different age groups. Eur J Health Res 2016;2:73-81.

9. Scarmeas N, Luchsinger JA, Stern Y, Gu Y, He J, DeCarli C, et al. Mediterranean diet and magnetic resonance imaging-assessed cerebrovascular disease. Ann Neurol 2011;69:257-268.










