Anticoagulants in Older Patients with Nonvalvular Atrial Fibrillation after Intracranial Hemorrhage
Article information
Abstract
Background and Purpose
Patients with nonvalvular atrial fibrillation (NVAF) who survive an intracranial hemorrhage (ICH) have an increased risk of ischemic stroke and systemic embolism (IS/ SE). We investigated whether starting oral anticoagulants (OACs) among older NVAF patients after an ICH was associated with a lower risk of IS/SE and mortality but offset by an increase in major bleeding.
Methods
We assembled a patient cohort from the Quebec Régie de l’Assurance Maladie du Québec (RAMQ) and Med-Echo administrative databases. We identified older adults with NVAF from 1995 to 2015. All patients with incident ICH and discharged in community were included. Patients were categorized according to OAC exposure. Outcomes included IS/SE, all-cause mortality, recurrent ICH and major bleeding after a quarantine period of 6 weeks. Crude event rates were calculated at 1-year of follow-up, and Cox proportional hazard models with a time-dependent binary exposure were used to assess adjusted hazard ratios (AHRs).
Results
The cohort of 683 NVAF patients with ICH aged 83 years on average. The rates (per 100 person-years) for IS/SE, death, ICH and major bleeding were 3.3, 40.6, 11.4, and 2.7 for the no OAC group; and 2.6, 16.3, 5.2, and 5.2 for OAC group, respectively. The AHR for IS/SE and death was 0.10 (95% confidence interval [CI], 0.05 to 0.21), 0.43 (95% CI, 0.19 to 0.97) for recurrent ICH and 1.73 (95% CI, 0.71 to 4.20) for major extracranial bleeding comparing OAC exposure to non-exposed.
Conclusions
Initiating OAC after ICH in older individuals with NVAF is associated with a reduction of IS/SE and mortality and a trend in recurrent ICH supporting its use after ICH.
Introduction
Atrial fibrillation (AF) is a cause of ischemic stroke (IS) and is expected to increase in prevalence in the coming years [1]. In addition, ISs associated with AF are more severe and carry a higher mortality rate [2]. Oral anticoagulant (OAC) therapy, either vitamin K antagonists (VKA) or direct oral anticoagulants (DOAC), has been shown to be efficacious in preventing ischemic events including strokes in AF [3-5]. However, one of the most feared and life-threatening complications of OAC therapy is intracranial hemorrhage (ICH) [6], and though the risk is less with DOACs, it is still present. This leads to a therapeutic dilemma which is to either avoid use of OAC in patients with AF after an ICH to reduce the risk of recurrent ICH or prescribe OAC to reduce the risk of IS or systemic embolism (SE). Present guidelines for ICH have not provided any clear recommendations because of a paucity of evidence in this area, and also by the lack of randomized controlled trials for this unmet need, since previous ICH was an exclusion criterion for all randomized clinical trials that tested anticoagulation in patients with AF [7,8].
However, recent observational studies [9-12], and meta-analyses [13-16] have suggested that the use of OAC after an ICH was associated with a reduction in all-cause mortality and ischemic events although in some reports [17,18], a higher rate of recurrent ICH was noted. Using Quebec healthcare databases, we evaluated the risk and benefits of OAC use after an ICH in older patients with nonvalvular atrial fibrillation (NVAF). We use timedependent modeling in order to relate recent and current exposure to OAC on the occurrence of events.
Methods
Data source
We assembled a cohort from administrative databases (hospital discharges [Med-Echo], medical services and public drug plan), administered by the Régie de l’Assurance Maladie du Québec (RAMQ). The databases were linked through encrypted health insurance numbers. Information from these databases provided a complete picture of hospital admissions. The protocol received the approval of the University of Montreal Ethics Committee.
Population-based cohort
From a random sample of 40% of a larger cohort for the period January 1, 1995 to December 31, 2015, we identified older individuals (over 65 years) who were discharged alive with a primary or secondary diagnosis of NVAF (International Classification of Diseases [ICD]-9 427.3, 427.31, 427.32, or ICD-10 I48).
The follow-up period for the cohort ended in December 2016. Patients with an incident ICH (ICD-9: 430, 431, 432.x, 852.x, 853.x; ICD-10: I60–I62, S063C, S064–S066) requiring admission to a hospital were included. Patients with an ICH or complication (ICD-9: 438.9; ICD-10: I690–692) in the 5 years before AF diagnosis were excluded. Patients needed to be on the RAMQ drug plan continuously for 12 months prior to the index ICH and during follow-up.
Patients were followed after a quarantine period of 6 weeks after hospital discharge for their ICH. This period was chosen to ensure that events during follow-up could reasonably be attributed to the treatment regimens rather than sub-optimal management of the initial coagulation abnormalities, or consequences from ICH complications. Patients on dual therapy (OAC and antiplatelet) or antiplatelet only were excluded.
Choice of the index date
The index date was defined as the date of the incident ICH (ICD-9: 430, 431, 432.x, 852.x, 853.x; or ICD-10: I60–I62, S063C, S064–S066). We then identified patients who filled a claim of warfarin or DOAC within 1 year after hospital discharge and who were living in the community. Patients were followed for 1 year or until the occurrence of the following censoring events: outcome, claim of antiplatelet dual-treatment, end of study or death, whichever came first.
Exposure to OAC treatment
At discharge from hospital and after the 6-week period quarantine, patients were classified by treatment regimens as OAC treatment (VKA/DOAC) or no OAC treatment. In order to investigate outcomes under different overall exposure levels, we categorized the patient population into three types: those who were treated continuously, variably, and never during the follow-up. Firstly, time-dependent exposures were defined firstly as a binary exposure variable, indicating the patient’s current exposure status (yes/no), and secondly as a categorical exposure variable indicating (1) a mean possession ratio (MPR) of ≥90% over the past 6 weeks; (2) MPR <90% over the past 6 weeks and exposed on the day of the event; (3) MPR <90% over the past 6 weeks and not exposed on the day of the event; or (4) never exposed over the past 6 weeks (reference). These two time-dependent exposures were evaluated at each week of follow-up, allowing for exposure to vary overtime for the same individual.
Outcome measures
The main analysis focused on the primary outcome including, IS/SE and all-cause mortality (Supplementary Table 1). Secondary analyses were performed separately for IS/SE, recurrent ICH, major extracranial bleeding, and all-cause mortality (Supplementary Table 1). We also reported the combination of IS/SE and recurrent ICH, the combination of death and recurrent ICH or the combination of death and major extracranial bleeding, as a global outcome measure reflecting clinical benefit, using the method proposed by Singer et al. [19]
Patient demographics and clinical characteristics
Comorbidities were ascertained at the time of ICH hospitalization. Other concomitant medications were defined as filled prescriptions up to 3 months before ICH hospitalization. The cardiovascular comorbidities and risk of stroke at baseline were evaluated with the CHA2DS2-VASc score [20,21], and we determined bleeding risk with a modified HAS-BLED score not including international normalized ratio (INR) lability [22] (Supplementary Table 2-4). We assessed comorbidities using the Charlson comorbidity index [23].
Statistical analyses
We used descriptive statistics for the demographics and clinical characteristics. For outcome analyses, events were identified and collected starting 6 weeks after hospital discharge for ICH. We depicted the overall 1-year risk of outcomes using Kaplan-Meier plots for three categories of patient exposure of the time over the total duration of follow-up (not exposed, variably exposed, and continuously exposed [MPR ≥90%]). The total duration of follow-up was calculated using the follow-up of each patient from baseline until IS/SE, recurrent ICH, major extracranial bleeding, and all-cause mortality or most recent censored follow-up assessment. The period at risk started at 6 weeks after the qualifying event and ended when patients experienced an outcome or the end of follow-up, whichever came first. We calculated crude event rates at 1 year by dividing the number of events occurring during follow-up with the person-years of follow-up for each treatment group (number of events per 100 person-years).
We used a Cox proportional hazards model with a time-dependent binary exposure to contrast the relative risks of an outcome for current OAC use (yes/no), estimating both crude and adjusted hazard ratios (AHRs). The baseline covariates in the adjusted analysis were selected based on the results of univariate and multivariable analyses and most relevant clinical variables (Supplementary Table 5 and 6).
A second model estimated AHRs for clinical outcomes with a time-dependent categorical exposure as defined above (Supplementary Table 7).
A third model estimated the crude and AHRs for all-cause mortality with the binary time-dependent exposure while also adjusting for time-dependent covariates IS/SE, recurrent ICH, and major extracranial bleedings (Supplementary Table 8). All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Sub-group analyses were performed for two sub-groups of ICH, spontaneous and traumatic to contrast the relative risks of an outcome between subjects on OAC treatment versus no OAC (sub-groups’ definition at the Supplementary Table 9). A sub-group analysis of patients older than 75 years was performed and compared to those under 75 years. The crude and AHRs were estimated using a Cox proportional hazards model with the binary time-dependent exposure.
Finally, we repeated the time-to-event analyses for the outcomes defined as a combination of IS/SE and ICH, death and ICH, and death and extracranial major bleeding, as respective global outcome measures reflecting overall clinical benefit were calculated using the method proposed by Singer et al. [19], and we provided 95% confidence intervals using the Bootstrap method.
Results
Demographics and clinical characteristics
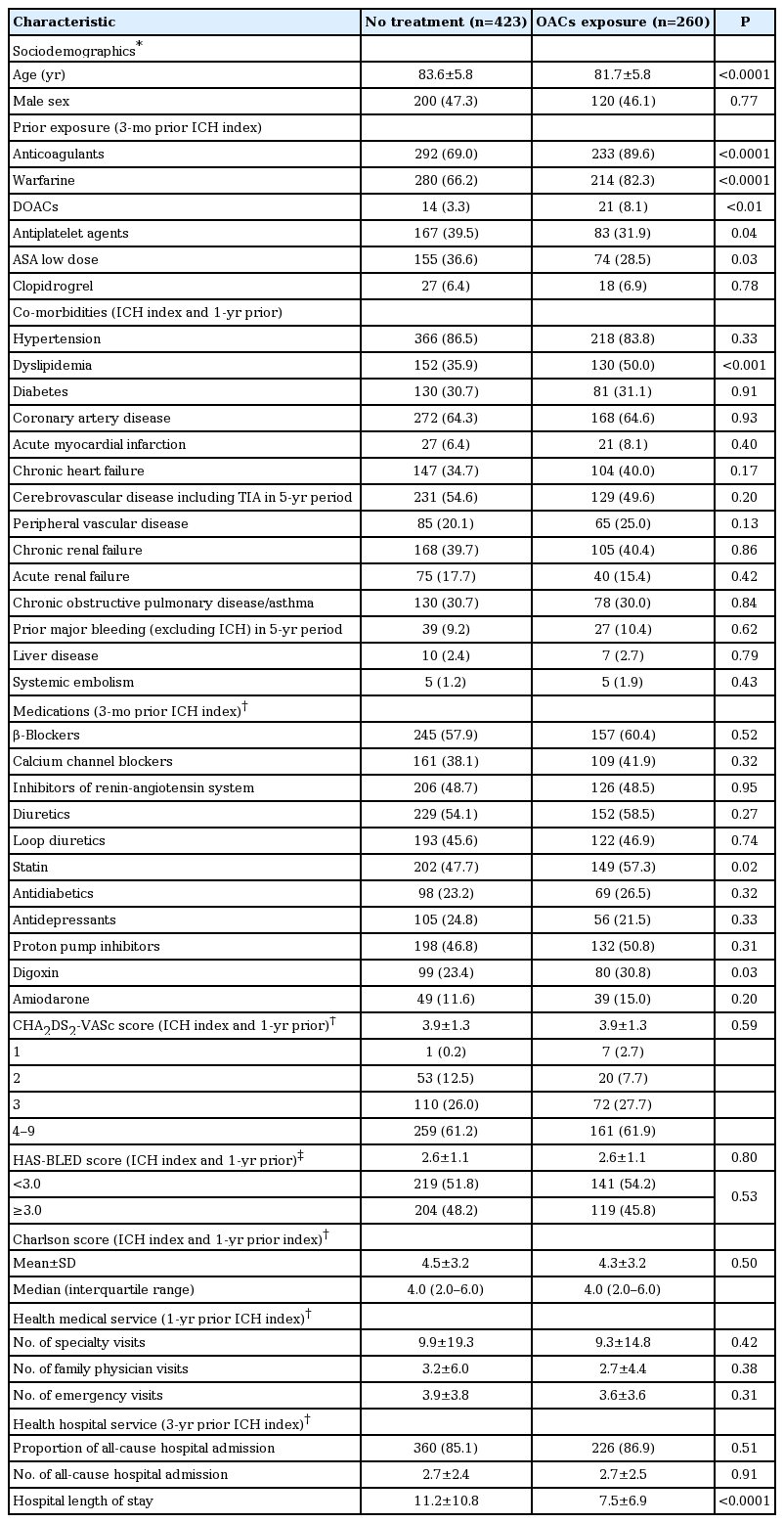
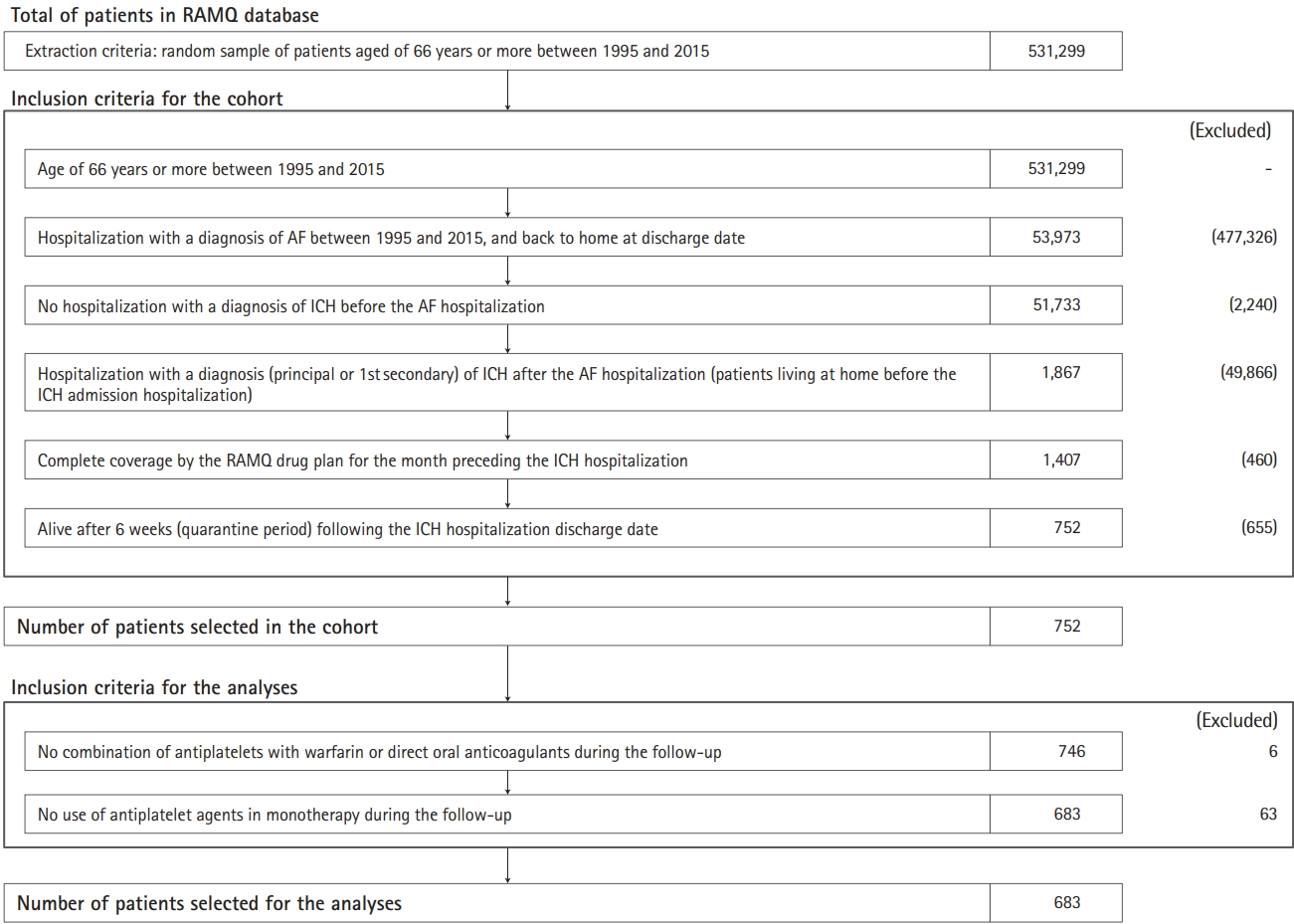
The cohort inclusion flow chart and patient characteristics are presented in Table 1 and Figure 1. Among 683 NVAF patients with ICH, 423 (61.9%) had no OAC exposure and 260 (38.1%) were exposed to OACs to some extent. Of the complete cohort, 148 (21.7%) were partially exposed and 115 (16.8%) were continuously exposed. Among the 260 patients who filled out an OAC prescription, 82.3% were initiated on warfarin, the mean age was 81.7 years, and 46.1% were men. In the same exposed subset, co-morbidities were as follows: ischemic heart disease (64.6%), hypertension (83.8%), heart failure (40.0%), diabetes (31.1%), dyslipidemia (50.0%), chronic renal disease (40.4%), peripheral vascular disease (25.0%), and previous stroke/transient ischemic attack (49.6%). Mean CHA2DS2-VASc and HASBLED scores were 3.9 and 2.6, respectively (Table 1). The patient characteristics according to OAC exposure categories were quite similar to those not exposed (Supplementary Table 10).
Exposure to OAC treatment
Among those who were exposed to OAC treatment, the proportions of patients exposed to several adherence levels defined as ≥90%, between ≥80% and <90%, between ≥70% and <80%, between ≥60% and <70%, and those <60% were at 44.6%, 11.9%, 8.5%, 7.3%, and 27.7%, respectively.
IS/SE and all-cause mortality
Median follow-up was 12 months. The Kaplan Meier curves for clinical outcomes during follow-up are presented in Figure 2. The overall unadjusted yearly rates for the primary outcome of combined end points of IS/SE and all-cause mortality for patients with any OAC exposure versus no exposure were 17.9 versus 43.1 per 100 person-years (Table 2). The Cox proportional hazards model with binary time-dependent exposure yielded an AHR 0.10 (range, 0.05 to 0.21) (Figure 3). The AHR for the categorical time-dependent exposure of ≥90% was at 0.10 (0.04 to 0.24), with similar results for the category of exposure <90% and being exposed at the time of event. In contrast, for the category of exposure <90% and not being exposed, the risk of IS/SE and all-cause mortality was significantly increased (AHR, 2.43 [1.56 to 3.78]) relative to no exposure.

Kaplan-Meier for outcomes during the 1-year period following hospital discharge. (A) Ischemic stroke or systemic embolism. (B) All-cause mortality. (C) Recurrent intracranial bleeding. (D) Major extracranial bleeding. SE, systemic embolism; OAC, oral anticoagulant; tx, treatment is defined as a variable or continuous exposure to OAC; Contin., continuous.
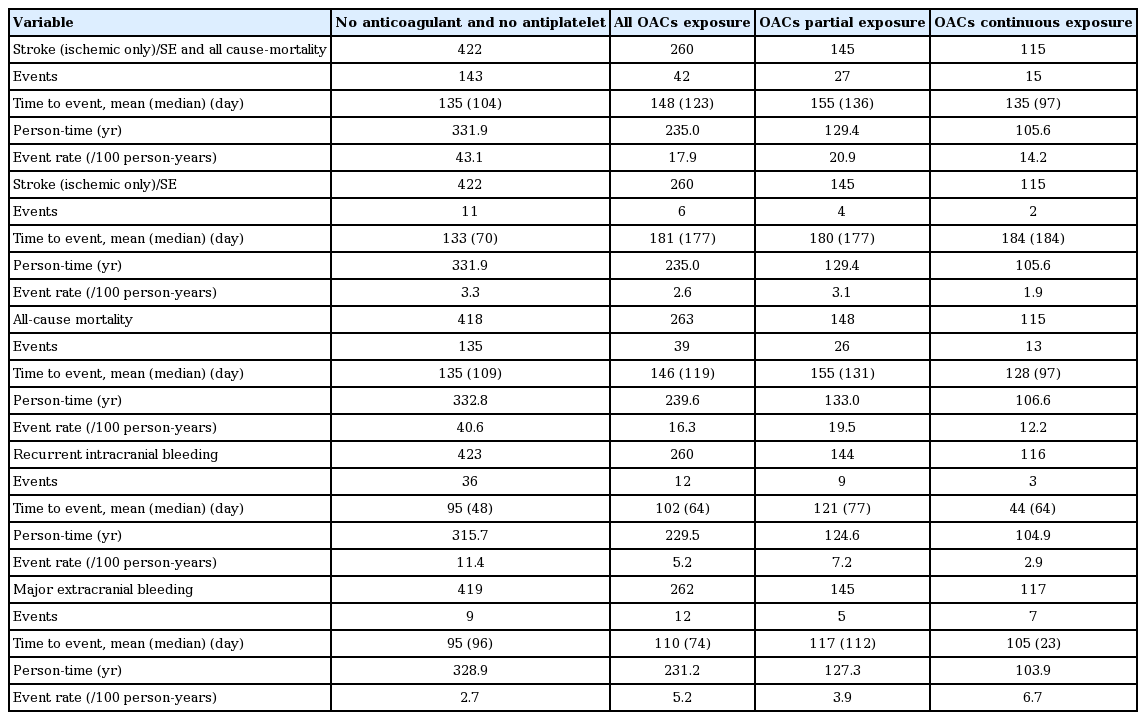
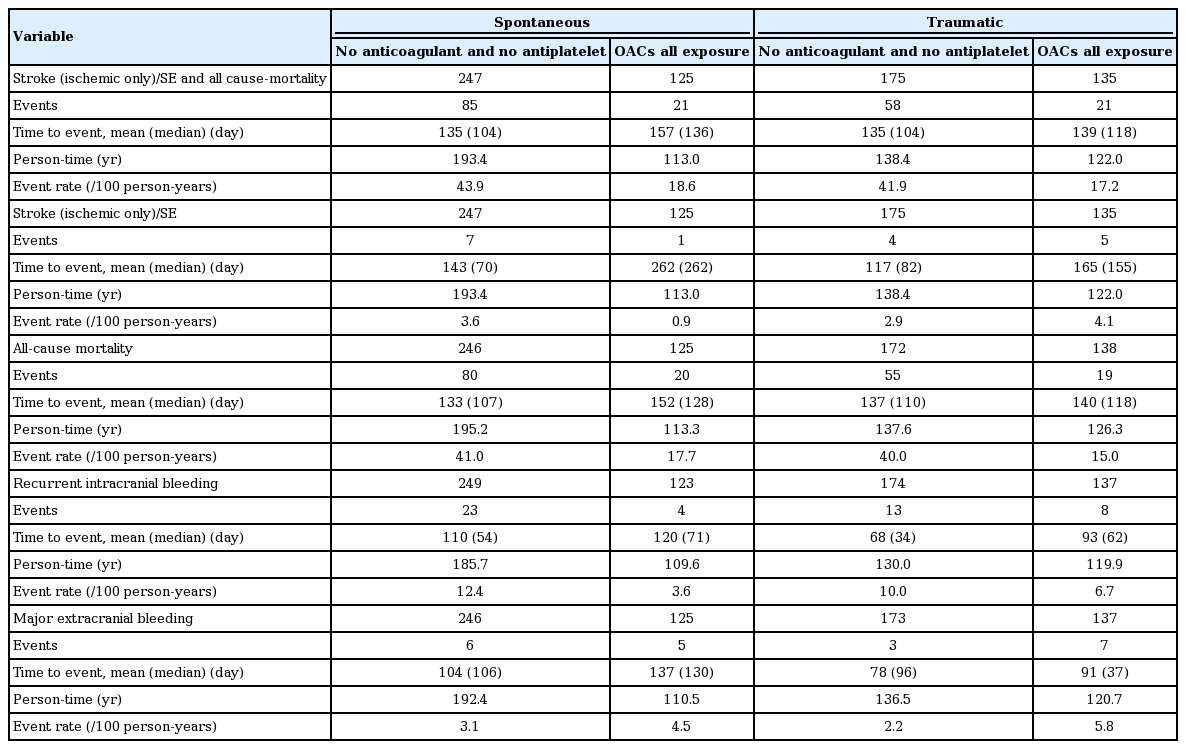
Rate of clinical events per categories of OAC exposure during 1-year period of follow-up for a quarantine period of 6 weeks

Forest plots of adjusted hazard ratios (AHRs) for binary exposure, and categorical exposure and being exposed or not exposed at the time of the event using time-dependent model during a 1-year of follow-up. OAC, oral anticoagulant; CI, confidence interval; SE, systemic embolism; BEV, binary exposure variable; CEV, categorical exposure variable; ICH, intracranial hemorrhage.
The overall unadjusted yearly rates for IS/SE for the group of any OAC exposure versus no exposure were 2.6 versus 3.3 per 100 person-years. As shown in Figure 2, the main model with binary time-dependent exposure yielded non-significant AHRs, as for all categorical time-dependent exposures. For all-cause mortality, any OAC exposure versus no exposure yielded 16.3 versus 40.6 per 100 person-years. The main model with binary time-dependent exposure gave an AHR 0.07 (0.03 to 0.17) (Figure 3). The AHR for binary and categorical time-dependent exposure of ≥90% was 0.04 (0.01 to 0.17), which is the range of the point estimate of the category of exposure <90% and being exposed at the time of event. In contrast, in the category of exposure <90% and not being exposed at the time of event, the risk of mortality was significantly higher (AHR, 2.43 [1.55 to 3.82]).
Finally, in the analysis where we adjusted for IS/SE, recurrent ICH and major extracranial bleeding, the estimated treatment effect of the binary time-dependent exposure was unchanged (AHR, 0.07 [0.03 to 0.17]) (Supplementary Table 8).
Recurrence of ICH and major extracranial bleeding
The unadjusted yearly rates for ICH recurrence for the group of any OAC exposure versus no exposure were 5.2 versus 11.4 per 100 person-years. The Cox proportional hazards model with binary time-dependent exposure yielded an AHR 0.43 (0.19 to 0.97) (Figure 3). The trend in the AHR for the categorical time-dependent exposure of ≥90% was 0.38 (0.13 to 1.08), close to that of the category of exposure less than 90% and being exposed at the time of event. And, in the category of exposure less than 90% and not being exposed at the time of event, the AHR was null (AHR, 1.00 [0.30 to 3.26]). But, for major extracranial bleeding risk, the group of OACs exposure versus no exposure was 5.2 versus 2.7 per 100 person-years; and, a trend of increasing risk can be observed across all the categories of OAC exposure.
Subgroup analyses
The rates of clinical events per exposure category are presented in Table 3. For spontaneous and traumatic ICH analyses, we used a time-to-event analysis to contrast the relative risks of an outcome between exposure groups. For spontaneous and traumatic ICH, AHRs for the composite of IS/SE and all-cause mortality for OACs exposure versus no OAC were 0.10 (0.04 to 0.27) and 0.11 (0.04 to 0.30), respectively; for all-cause mortality, those estimates were 0.08 (0.03 to 0.25) and 0.06 (0.01 to 0.23); for recurrent ICH, those estimates were 0.34 (0.10 to 1.14) and 0.53 (0.18 to 1.60); and for major extracranial bleeding, those estimates were 1.67 (0.48 to 5.79) and 1.66 (0.46 to 5.97), respectively (Supplementary Table 11). Finally, we still observed similar results for the sub-group of patients older than 75 years old (Supplementary Table 12).
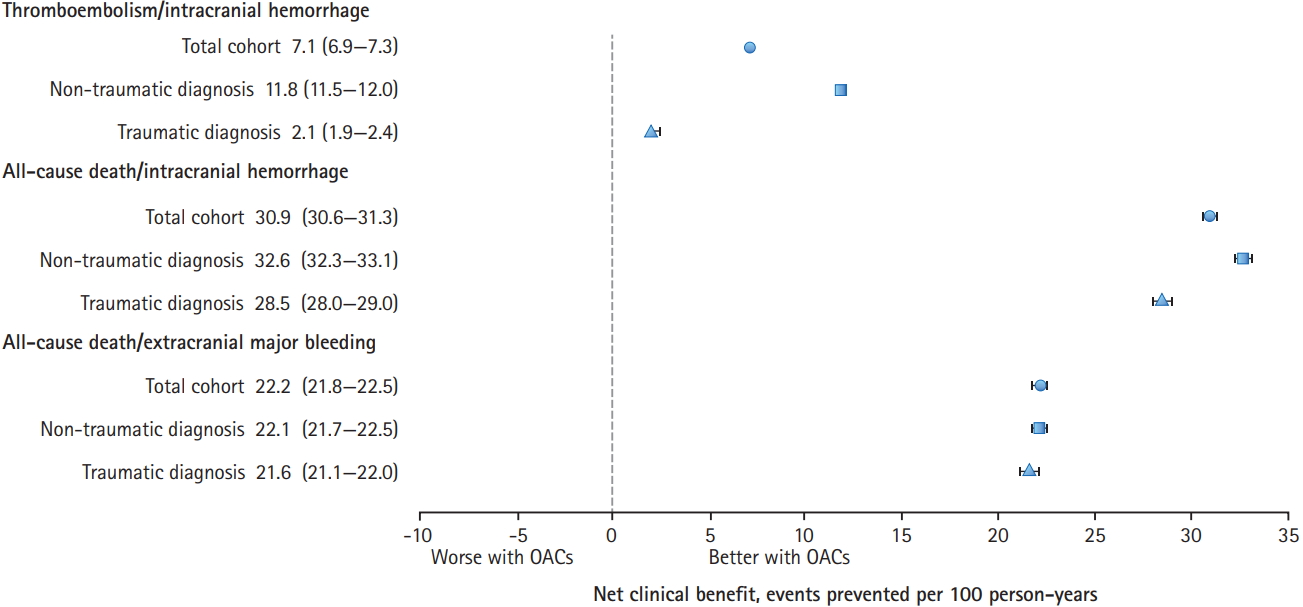
Net clinical benefit
The adjusted net clinical benefit for OACs exposure for the total cohort, and broken down into spontaneous or traumatic ICH are depicted in Figure 4 and the Supplementary Table 13-Supplementary Table 15. The OAC exposure is associated with a better net clinical benefit.
Discussion
In this study of older individuals diagnosed with NVAF who experienced an ICH, our main findings include (1) a high adherence level of OAC after an ICH was significantly associated with a reduction in the combined outcome of IS/SE and allcause mortality; (2) all-cause mortality as a single outcome was significantly lower for those with high OAC adherence level in contrast with IS/SE events; (3) no significant difference was observed between the two sub-groups of spontaneous ICH or traumatic ICH; (4) similar results were observed the subgroup of patients older than 75 years; (5) the risk of major extracranial hemorrhages was not significant but the point estimate suggested a trend in increased risk among OAC groups; and (6) the net clinical benefit which included all IS/SE and recurrent ICH showed a significant benefit in favor of OAC treatment when compared to the no OAC group, and the estimated benefits were even more extreme for the outcomes of all-cause mortality and recurrent ICH or major extracranial bleeding.
Our finding of significantly lower IS/SE and all-cause mortality as a combined outcome in regularly OAC treated NVAF individuals after an ICH is similar to previous recent reports [10-12,15-17]. In our study, this beneficial effect appears to be mostly driven by a strong reduction in mortality rather than by a reduction in IS/SE. Similar to our own results, two other studies [10,17] reported a non-significant reduction in IS/SE. This in part may possibly be due to the smaller number of IS/SE versus death in these populations; as an example, in the study by Nielsen et al. [17] mortality events were more than five times more frequent than thromboembolic events and in our own study they were 10 times more frequent. This explanation is also indirectly supported by the study of Chao et al. [9] in which the beneficial effect of OAC therapy in preventing IS as a single outcome was based on a very large number of cerebral ischemic events (n=1,094).
Similar to previous studies [9,11,13], we found no significant difference in outcomes for the sub-group of spontaneous ICH compared to traumatic ICH, although this differs from the report by Nielsen et al. [17], in which resumption of OAC therapy was associated with a reduced risk of recurrent ICH in the traumatic ICH group only. As well, another study [10] reported a significant reduced risk for recurrence of ICH for patients treated with OAC if the quarantine period was 4 weeks or less after ICH hospitalization. A potential explanation for this finding could be that patients on an OAC have more regular medical follow-ups related to their need for control of anticoagulation (INR) and consequently better control of relevant risk factors such as hypertension which could in turn result in a reduced risk of recurrent ICH. Alternatively, imbalances of unmeasured variables which could be linked with a higher likelihood of OAC treatment and smaller risk of ICH recurrence (size and location of ICH) could lead to confounding bias. Again, only a minority of patients were prescribed OAC treatment, and it is likely that these patients may be at higher risk of IS/SE or lower risk of recurrent ICH compared to those not exposed. The severity of ICH could bias the association with resumption of OAC treatment by the indication bias. And, the patients having extracranial major bleeding seem to have more comorbidities, as suggested by crude and AHRs (Supplementary Table 5 and 6). Finally, the relative proportion of spontaneous vs traumatic ICH within the ICH population studied could influence results if both groups don’t present the same inherent recurrence risk for ICH.
In addition, we decided to include as an outcome the combination of IS/SE and recurrent ICH, all cause of death and recurrent ICH, and all-cause of death and extracranial bleeding based on the concept of net clinical benefit [19]. We evaluated the risk-benefit balance in this population which is at a high risk of both disabling and lethal ischemic as well as ICH or extracranial major bleeding events. Based on the adjusted net clinical benefit for OAC exposure for the total cohort, and also broken down into spontaneous or traumatic ICH, we found better net clinical benefits in favor of the OAC treatment compared to not being exposed.
In contrast to previous studies, we included time-dependent categorical exposure groups which consider the recent history of OAC exposure. Globally, partial recent exposure and not currently being exposed did not show any significant benefit for any of the outcomes, when compared to the no OAC exposure group. This observation suggests that the benefits of OAC treatment can be achieved through OAC adherence or a more optimal patient management of OAC exposure. We choose not to include patients treated with antiplatelet agents since previous randomized trials [24] and observational studies [9,10] did not report any benefit for these agents.
Our study presents several positive aspects, some of these include a relatively large and well characterized Canadian population-based cohort, inclusion of time-dependent categorical OAC treatment exposure groups during the followup that better characterize real life, and the inclusion of net clinical benefit outcomes which represent a more meaningful picture of the balance between risk and benefit for OAC treated individuals. However, our study has several limitations. First, this observational study using hospital administrative data which does not include all clinically relevant variables (INR stability, functional status, or risk of falls). Second, we had no access to neuroimaging studies to characterize certain relevant clinical variables such as the location (deep vs. lobar) and volume of the ICH, and the presence of specific abnormalities like micro-bleeds which could influence antithrombotic management [25]. Third, there is also a possibility based on clinical and imaging data that the patients receiving OAC therapy were deemed to be at higher risk of IS/SE or lower risk of recurrent ICH compared to those not exposed. Four, our results may not be generalizable to other groups such as non-hospitalized individuals with NVAF and other ethnic groups as our population was mostly white [26]. Our results would only partly apply to DOACs as we only had a small number of individuals treated. Finally, residual bias is possible in regards to unmeasured variables and the healthy population effect.
Conclusions
In summary, our results support the use of OAC in older patients with NVAF after an ICH, with the benefit of preventing mortality and ischemic events offsetting the risk of ICH recurrence. There is need for risk stratification for the sub-type of stroke, localization and severity of ICH and OAC exposure level. Giving, that this cohort study may have the residual risk for unmeasured confounding future randomized controlled trials [27] are required to confirm our results.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2018.02243.
Definition of variables outcomes according to ICD-9 and ICD-10 from Med-Echo databases
Risk score definition for CHA2DS2-VASc and Modified HAS-BLED
Definition of variables used in the risk score definition of CHA2DS2-VASc according to ICD-9 and ICD-10 from Med-Echo databases
Definition of variables used in the risk score definition of HAS-BLED based on associated morbidities and concomitant drug
Crude hazard ratios of clinical outcomes with a quarantine period of 6 weeks with binary time-dependent exposure (full cohort)
Adjusted hazard ratios of clinical outcomes with a quarantine period of 6 weeks with binary time-dependent exposure (full cohort)
Adjusted hazard ratios of clinical outcomes with a quarantine period of 6 weeks with binary time-dependent exposure and categorical exposure
Adjusted hazard ratios of all-cause mortality with a quarantine period of 6 weeks with binary time-dependent exposure and timedependent covariates
Definition of subgroup analysis (e.g., spontaneous and traumatic ICH) [17]
Baseline characteristics of full cohort for a quarantine period of 6 weeks according drug exposure categories
Crude and adjusted hazard ratios of clinical outcomes with binary time-dependent exposure in the spontaneous and traumatic ICH
Crude and adjusted hazard ratios of clinical outcomes with binary time-dependent exposure in the age population older ≥75 and <75 years
Net clinical benefit of the combination of ischemic stroke and systemic embolism and ICH
Net clinical benefit of the combination of death and ICH
Net clinical benefit of the combination of death and extracranial major
Notes
Disclosure
Sylvie Perreault is holding the Sanofi Canada endowment Research Chair in Optimal Drug Use.
Acknowledgements
The study was funded by the Heart and Stroke Foundation of Canada.
We thank the RAMQ and Quebec Health Ministry for assistance in handling the data and the Commission d’accès à l’information for authorizing the study.