Stroke Epidemiology in Thailand
Article information
Abstract
Stroke is a major health burden in Thailand. It is the leading cause of death and long term disability in both men and women. Despite the improvement of healthcare system, the mortality rate of stroke is still increasing during the past 5 years. The incidence of stroke in Thailand is now being studied in a large population based cohort. The prevalence of stroke is estimated to be 1.88% among adults 45 years and older. Stroke is more prevalent in men than in women and the mean age of stroke onset is 65 years. Hypertension, diabetes, dyslipidemia, metabolic syndrome, and atrial fibrillation are major risk factors of stroke in the Thai population. Evolution from predominantly rural to urbanized industrial communities result in the increasing prevalence of these risk factors. Similar to other parts of the world, ischemic stroke is the most common stroke type but the proportion of hemorrhagic stroke is higher when compared to Caucasian populations. Among patients with ischemic stroke, lacunar stroke is most common, accounting for almost half followed by atherosclerotic disease. Intracranial atherosclerosis is also prevalent in Thai population. For acute treatment, intravenous thrombolysis has been used in Thailand for over 20 years. Its cost is reimbursed by the national health care system but its use is still limited. With the introduction of the stroke fast track system, prompt stroke treatment across the country is warranted. Stroke unit is now the standard of care in large regional and provincial hospitals.
Introduction
Thailand is a country located in South-east Asia with an approximate current population of 67 million people. The total area of the country covers around 514,000 square kilometers which is similar in size with Spain. Thailand's tropical climate is generally hot and humid from March to November and very mild during the cooler seasons. Thai ethnics (75%) make up the majority of the population whereas those with Thai Chinese backgrounds account for 14%. Ninety-five percent of the population is Buddhist which is also the official religion. Life expectancy of the total population at birth is 73.83 years (71.45 years in male and 76.33 years in female). With a low population growth rate of 0.543% and an increase in life expectancy, Thailand's aging population is proportionally increasing.1
The Thai Ministry of Public Health has divided Thailand into 13 geographical areas. Each area covers a population of approximately 5 million with about 5,000 hospital beds. There are approximately 12,000 physicians in Thailand. Roughly, the physician to population ratio would be one physician to 5,500 people. Currently, Thailand has about 300 active neurologists. However, more than two-thirds of this specialized group resides in the greater Bangkok metropolitan area and other neighboring provinces. Therefore, the concentrated grouping of neurologists in Bangkok reveals that there is a shortage of neurologists across the country, especially in rural areas including the Northeastern and Southern parts of Thailand.
Thailand, similar to most developing countries, has undergone significant economic and health transitions. It has gradually changed from a traditional agricultural base to that of a flourishing industrialized system. The shift from a predominantly rural community to an urbanized one has changed many lifestyle preferences as well. As a result, diet and physical activities have undergone complete transformations from healthy diets consisting of mainly rice and vegetables to more westernized diets that are rich in fat and sugar. Moreover, urbanization has led to greater competition in the community and less time at home. Family roles have shifted and traditional home cooked meals have been replaced by the convenience of fast food. Physical activity of the population has also progressively declined giving way to increased time of sedentary activities.2,3 As a result, the incidence of cardiovascular diseases, particularly stroke, has increased.
As the leading cause of death and disability in Thailand, it is estimated that, there are more than 250,000 new stroke cases each year. Stroke claims approximately 50,000 lives annually.3 Alarming statistics from the Ministry of Public Health, rank stroke the first most common cause of death among both women and men. Stroke related mortality is unfortunate but for survivors, stroke creates major burdens of disability for patients and their families. It carries the highest rank for disease burden in Thailand measured by disability-adjusted life years (DALYs) lost in female and the third in male.4
Epidemiological data of stroke in Thailand can be gathered from 2 main sources. First, general data collected from hospitals and the national health security service are reported in the official Country Report from the Ministry of Public Health. A Second more accurate data source comes from national surveys, registries, and cohort studies. A large cohort study among more than 20,000 Thais in various parts of Thailand or the Thai Epidemiological Stroke (TES) Study has provided salient data related to stroke prevalence and it is also the first study offering data on the incidence of stroke in Thailand.5 Another study worth mentioning is the Thai Stroke Registry which has collected data from more than 1,000 stroke patients who were admitted to 76 hospitals around Thailand.6 Information regarding risk factors and treatment are derived from other smaller studies.
Stroke mortality
Stroke is the first leading cause of death in Thailand in both men and women. According to the Ministry of Public Heath in Thailand, there are more than 50,000 deaths from stroke annually.1 WHO data in 2004 reported that the age-standardized death rate per 100,000 for cerebrovascular disease in Thailand is 100.7 The finding that stroke causes more deaths than ischemic heart disease is consistent with the cardiovascular disease mortality pattern of East Asian countries.8
A large retrospective study of all-cause mortality among patients with cardiovascular diseases in Thailand was conducted in 2011. This study extracted data from the national database through the Central Office for Healthcare Information in 98,486 Thai patients. These patients were admitted in government hospitals due to established cardiovascular diseases (acute coronary syndrome, ischemic stroke, peripheral artery disease, congestive heart failure or atrial fibrillation). Nearly a quarter of the patients, 25,813, suffered from acute ischemic stroke in this study. Interestingly, it was found that stroke was the third leading cause of hospital admission among cardiovascular diseases with an in-hospital mortality rate of acute stroke of 11.9%.9
More information regarding in-hospital mortality of stroke was sourced from the Thai Stroke Registry where 1,222 acute ischemic stroke patients were prospectively registered throughout the country during 2008-2009. The data were collected from 3 different hospital levels; university, regional, and community hospitals. In this particular study, the in-hospital death rate was only 3.2%.6 The low mortality at the time of discharge in this study might be explained by a rather low median length of stay (4 days) and the type of participating hospital itself. Since hospital selection in the registry was voluntary, data from non-participating centers possibly with lower standards of care were not available.
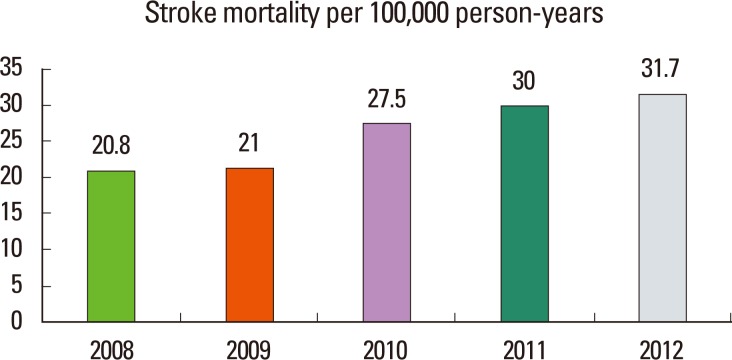
According to the data from the Ministry of Public Health, the mortality rate of stroke in Thailand is increasing during the past 5 years. The mortality increased from 20.8 in the year 2008 to 30.7 per 100,000 populations in the year 2012. This may reflect the increased incidence of stroke in the country.10 Figure 1 demonstrates the stroke mortality per 100,000 population according to data from the Ministry of Public Health.
Stroke incidence
To date, there is little information on the incidence of stroke in Thailand. It is currently being studied in a large cohort called the Thai Epidemiological Stroke (TES) Study. This study has collected data from over 20,000 subjects from the 5 major geographical regions of the country.5
Among the world population, age-adjusted stroke incidence rates in high-income countries have decreased from 163 per 100,000 person-years from 1970-1979 to only 94 per 100,000 person-years from 2000-2008. In contrast, the incidence of stroke has nearly doubled in low- to middle-income countries. (52 per 100,000 person-years to 117 per 100,000 person-years, respectively).8 As a middle income country, it is believed that the stroke incidence in Thailand will follow this rising trend. The incidence of stroke is projected to increase as the Thai population ages and although further study is needed to support this projected trend, it is still approximated that at least one new stroke case occurs in Thailand every 2 minutes.
Stroke prevalence
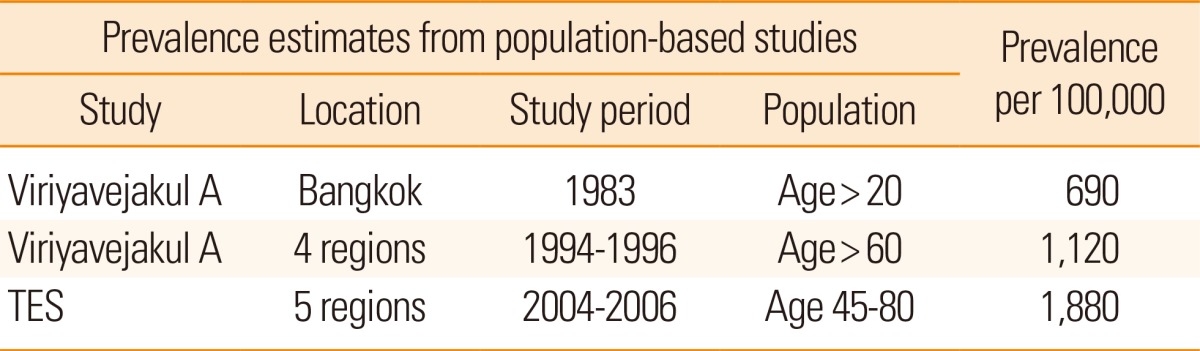
The earliest prevalence study on stroke in Thailand was published in 1983. This study included subjects in the Bangkok metropolitan area who were over 20 years of age. It showed that the prevalence of stroke was 690 per 100,000 persons.11 Another study among 3,036 elderly Thais over 60 years old in 4 geographical regions of the country conducted during 1994-1996 revealed a 1.12% prevalence of stroke with the highest prevalence found in the central region of Thailand.12
The most recent Thai Epidemiological Stroke Study found that the prevalence of stroke in populations over the age of 45 is 1.88%. Men had a higher prevalence of stroke than did women in all age groups. Stroke prevalence differed among the five geographic regions of the country with the highest prevalence in the capital city, Bangkok (3.34%) followed by central (2.41%), southern (2.29%,), northern (1.46%), and north-eastern regions (1.09%). A number of factors associated with higher stroke prevalence were also identified as older age, male gender, occupational class (manual class and unemployed), history of hypertension hypertension, diabetes mellitus and hypercholesterolemia.5 In this particular study, the stroke prevalence was higher than those reported in previous studies in Thailand but still remains lower than that of developed countries, which may relate to the number of case fatalities. Summary of the studies of stroke prevalence in Thailand is shown in Table 1.
Risk factors
Age
Stroke occurs at any age but it is mainly a disease of the elderly. According to the Thai Stroke Registry, the mean age of patients at the onset of ischemic stroke in Thailand is approximately 65 years.6 This age is similar to findings from previous reports from developing countries.13-15
However, the onset of stroke in Thai patients is earlier than those in developed countries.16-22 This may be due to poorly controlled vascular risk factors in the Thai population. The stroke prevalence by age group is shown in Figure 2.
Hypertension
Hypertension is very common in the general population especially among the elderly. Data from the 2009 multistage cross-sectional Fourth National Health Examination Survey (NHES) of 18,629 Thai adults over the age of 20 years revealed that the prevalence of hypertension in Thailand is 21%.23
Hypertension is the most common and well established risk factor of stroke in most studies. In the Thai Stroke Registry, hypertension was found in 53% of the cases.6
Stroke risk factors focusing on hypertension were recently studied in a multicenter observational study between February 2010 and January 2011 at 24 selected stroke hospitals (8 academic hospitals, 9 regional referral center hospitals, and 7 provincial and other hospitals) in 6 geographical regions across Thailand. Self-reported hypertension prior to stroke was found in 62.5% of the patients. During acute periods of stroke, as expected, most patients with high blood pressure were not treated with antihypertensive agents. Surprisingly, only 49.1% of 558 stroke patients had good control of their blood pressure at 120 days after stroke. Therefore, more effort is still needed to increase the awareness of hypertension among physicians and patients in order to achieve a better control of blood pressure in the Thai population.24
Diabetes
According to the Fourth NHES, the age-adjusted prevalence of diabetes was 7.5% in adults over the age of 20 years. Among patients with diabetes, about one-third were undiagnosed. The prevalence of impaired fasting plasma glucose in the same population was 10.6%. Higher prevalence of diabetes was found in women, aging populations, and those who live in urban areas. The prevalence of diabetes has slightly increased from 2004 to 200925 and was significantly higher in women than in men (8.3% vs. 6.6%). In a cross-sectional, multi-center hospital-based diabetes registry among 9037 diabetic patients in Thailand, the Thailand Diabetes Registry Project, stroke was found in 3.5% of diabetic patients.26 According to the Thai Stroke Registry, diabetes was found in 26% of stroke patients.6
Metabolic syndrome
The prevalence of metabolic syndrome in the Fourth NHES was 23.2% among adults aged 20 years or older, and was substantially higher in women than in men (26.8% in women compared to 19.5% in men). Among men, the prevalence of metabolic syndrome in urban areas was higher than those in rural areas, whereas in women, metabolic syndrome was more prevalent in rural areas than in urban areas.27
Obesity is also a rising health problem among Thais. According to the Fourth NHES, 35% of men and 44.9% of women were overweight with BMI≥23 kg/m2 using the Asian cut-points. Age was positively associated with being overweight in both genders.3
Smoking
Due to strong support and efforts by the Thai government to educate the public about the adverse effect of smoking, the smoking rate of the Thai population has steadily declined. According to the Ministry of Public Health, only 18.4% of Thais smoke. By gender, 36% of men are smokers while only 1.6% of women are smokers.
Dyslipidemia
Dyslipidemia especially defined as elevated low density lipoprotein cholesterol (LDL-C) is known to be a risk factor of atherosclerosis related ischemic stroke. According to the Thai Stroke Registry, hypercholesterolemia was found in 30% stroke cases.6 However, the prevalence of dyslipidemia was much higher in a single center hospital based study at our King Chulalongkorn Memorial Hospital where 80% of patients with ischemic stroke had a high LDL-C level of more than 100 mg/dL.
Atrial fibrillation
Atrial of fibrillation (AF) is a common problem especially among elderly. AF was found in 10% of patients who presented with acute ischemic stroke at King Chulalongkorn Memorial Hospital. Data from a retrospective study among patients who were diagnosed with AF and presented to the ambulatory care clinic at a university hospital in 2008 demonstrated that 52.8% of patients at intermediate risk and 70.3% patients at high risk according to CHADS2 score were prescribed warfarin. In the high risk group, 19.6% received only antiplatelets and 10.1% received no antithrombotic therapy.28
Stroke types and subtypes
Ischemic stroke is the major type of stroke in Thailand. However, when compared to Caucasian populations, there is a higher proportion of intracerebral hemorrhage. According to hospital based data, hemorrhagic stroke accounts for about 20% of all stroke cases.
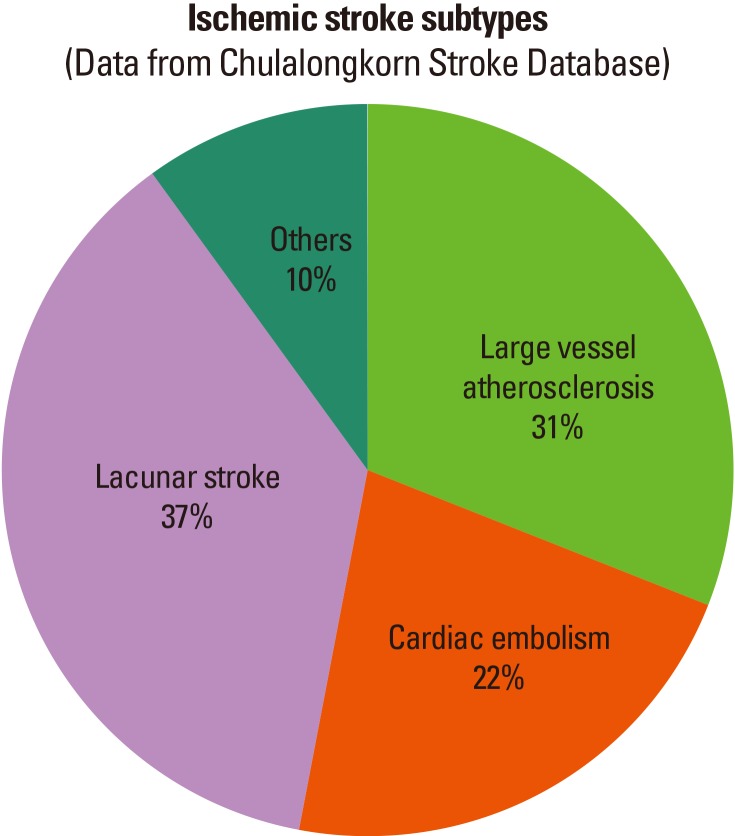
Among patients with ischemic stroke, lacunar infarction is the most common subtype followed by large artery atherosclerosis, and cardioembolism. Similar to the findings among other East Asian and Southeast Asian countries, significant carotid atherosclerosis was found in only 11% of patients. In contrast, intracranial atherosclerosis was found more frequently, accounting for 23% of the cases. Furthermore, the number of patients with intracranial atherosclerosis is likely to be even higher since some of them may present clinically as lacunar infarction where sometimes CT scan is the only diagnostic imaging modality. The subtypes of stroke in Thailand from Chulalongkorn stroke database is demonstrated in Figure 3.29
Stroke care in Thailand
Intravenous thrombolysis with recombinant tissue plasminogen activator is now the standard treatment for patients with acute ischemic stroke and is recommended by the Thai Stroke Guidelines. The first patients ever treated with intravenous thrombolysis was in 1996 and later on, the stroke fast track program was developed, initiated, and implemented by and at King Chulalongkorn Memorial hospital.30,31 The stroke fast track program is a hospital system designed to allow medical triage personnel at the hospital to identify patients with stroke early on in order to take proactive measures for prompt investigation and management with the stroke team. Leading to a higher number of acute stroke patients receiving intravenous thrombolysis within the critical window of time, the stroke fast track system has proven successful. At present, the fast track system has been adopted by many other university hospitals as well as regional, provincial, and some community hospitals.
For all Thai citizens, treatment costs can be reimbursed from the Universal Coverage Program provided by the National Health Security Office. According to the Ministry of Public Health, the proportion of patients receiving intravenous thrombolysis among those with acute ischemic stroke or acute stroke in Thailand has increased from 0.38% in 2008 to 1.95% in 2012. Although this figure is encouraging, one significant gap in acute stroke care is public education regarding stroke warning signs and act on stroke in Thailand.
The Stroke Unit is a critical component towards the betterment of stroke care in the country.32 Current data show that there are more than 110 stroke units across Thailand, mostly in regional and provincial hospitals. However, according to the Thai Stroke Registry, only one-fourth of patients were admitted to a specialized acute stroke care unit. The proportion of stroke unit admission was higher in university hospitals (50%) compared to 17.1% and 3.4% in regional and community hospitals, respectively. In the acute period, most ischemic stroke patients received aspirin within 48 hours of admission (71%).
As for secondary stroke prevention, antiplatelet was used in 80% of the cases. High rates of statin treatments were also noted. Seventy-three percent of patients received statin on discharge. After discharge, most Thai patients return home and are taken care of by family members. There are very few patients placed in nursing care facilities. This is due to cultural influences of Thai families where large extended families provide care for ailing family members.
In conclusion, stroke is a major health burden in Thailand. It is the leading cause of death and long term disability. The incidence of stroke in Thailand is now being studied in a large cohort. The estimated prevalence of stroke is 1.88% among adults 45 years and older. Stroke is more prevalent in men and the mean age of stroke onset is 65 years. Hypertension, diabetes, dyslipidemia, metabolic syndrome, and atrial fibrillation are major risk factors of stroke in the Thai population. Significant economic and health transitions from predominantly rural to urbanized communities may be responsible for the increasing prevalence of these risk factors. Similar to other parts of the world, ischemic stroke accounts for the majority of strokes but there is a higher proportion of hemorrhagic stroke when compared to Caucasian populations. Among patients with ischemic stroke, lacunar stroke accounts for almost half followed by atherosclerotic disease. Intravenous thrombolysis has been used in Thailand for over 20 years. Its cost is reimbursed by the national health care system but its use is still limited. With the introduction of the stroke fast track system and acute stroke unit, prompt stroke treatment across the country is ensured.
Notes
The authors have no financial conflicts of interest.