Occupational Risk Factors for Stroke: A Comprehensive Review
Article information
Abstract
For primary prevention, it is important for public health and clinical medicine to identify and characterize modifiable risk factors of stroke. In existing literature, the impact of occupational variables on ischemic and hemorrhagic stroke has been extensively studied. This review summarizes the available data on the significance of occupational variables in stroke. The results of this review suggest that there is sufficient evidence for the relationship between increased risk of stroke and job stress, working in extreme temperatures, long working hours, and/or shift work. The association between long working hours and occupational exposure to noise and chemicals remains inconclusive although several studies have reported this finding. This review will act as a step toward future research and provide information that may serve as a baseline for developing targeted interventions to prevent stroke in the working population.
Introduction
Stroke is the leading cause of long-term disability among adults and the second most common cause of death globally, making it a major public health concern [1]. Although high-income countries have achieved significant reductions in cerebrovascular disease incidence and mortality, low-income countries still have a long way to go [2].
Many countries have struggled to prevent or improve the outcomes of patients with stroke. One is to reduce the risk factors of stroke through health education or by promoting prevention through social media. Along with ischemic heart disease, stroke has definite risk factors; 90% of stroke have 10 risk factors [3,4]. Generally, risk factors for stroke can be divided into non-modifiable risk factors, such as age and sex, and modifiable risk factors, such as high blood pressure, diabetes mellitus, dyslipidemia, atrial fibrillation, and smoking [4]. According to estimates of the Global Burden of Disease Study, 33.4% of the stroke burden (as measured in disability-adjusted life-years, DALY) was attributable to potentially modifiable environmental and occupational risk factors, globally [5]. Therefore, reducing exposure to these factors should be prioritized to reduce stroke burden in many countries.
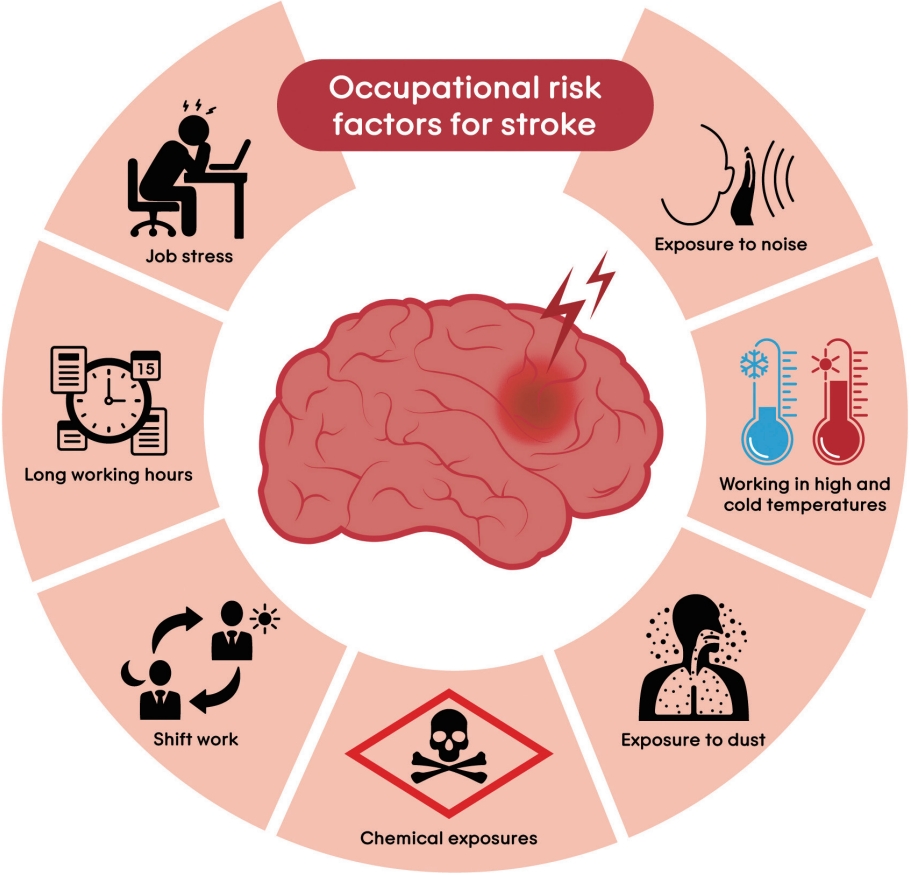
Several risk factors are intricately interconnected and not independent of a particular work setting. Recent studies have shown that overtime correlates with unhealthy behaviors such as smoking, alcohol-use, inactivity, inadequate sleep [6], and chronic diseases [7]. Aside from well-known risk factors, job-related factors are also considered modifiable risk factors for stroke, including shift work and long working hours, job stress, physical conditions such as noise and extreme temperatures, as well as exposure to dust and chemicals such as metals and carbon disulfide (CS2) (Figure 1). Numerous epidemiological studies reported that the workplace is an important focus area for stroke prevention and management.
Clinically, when evaluating and treating stroke, the etiology is considered the most important factor, especially for ischemic stroke. Various clinical examinations aim to differentiate the etiology. The Trial of ORG 10172 in Acute Stroke Treatment (TOAST) classification is the most common classification for identifying etiology and is largely divided into large artery disease (LAD), small vessel disease (SVD), and cardioembolic (CE) stroke. Conventional vascular risk factors or metabolic syndromes accelerate atherosclerosis and are associated with LAD and SVD, whereas causes of atrial fibrillation (AF), flutter, and heart failure are associated with CE stroke. If clinicians cannot identify the etiology, they may suspect drug-related, occupational, or environmental factors. Regarding occupation, AF is relatively common in athletes [8], whereas patent foramen ovale is common in divers [9,10].
Therefore, this review aimed to examine the available evidence on the role of occupational factors in stroke. This will pave the way for further investigation and provide fundamental knowledge for formulating targeted interventions to prevent stroke in the working population.
Evidences in previous research
Job stress
Job stress occurs when the requirements do not match a worker’s skills, resources, or needs; thus, leading to negative physical and emotional reactions [11]. The job strain model, also known as the demand-control model (DCM), is one of the most commonly used theoretical models in epidemiological research. DCM emphasizes situational workplace features, such as psychological job demands and control, as well as how these affect worker health and lifestyle [12]. Time constraints, cognitive demands, and responsibilities to multitask are all examples of psychological demands of the workplace, whereas job control refers to how workers influence decisions at work. Job demand and control combinations created four work situations: active (high demand and high control), job strain (high demand and low control), passive (low demand and low control), and low strain (low demand and high control). Job strain is the most stressful scenario because it limits autonomy and control, while the pressure is constant, thus impeding effective coping [13]. In developed countries, approximately 20%–25% of employees are exposed to job strain [14]. Chronic stress at work affects all body systems, including the cardiovascular system, and can lead to many diseases.
There is extensive evidence that workplace stress may increase cardiovascular disease (CVD) risk [15]. However, relatively little is known about whether job stress is linked to the risk of stroke because only a few studies have focused on stroke as a specific CVD outcome with unclear findings. Huang et al. [16] conducted a meta-analysis to investigate the relationship between job strain and risk of incident stroke. Six prospective cohort studies comprising 138,782 participants found that high-strain jobs increased the risk of stroke, especially among women. Around the same time, an individual-participant-data meta-analysis of 190,000 working males and females in Europe was conducted [17]. The results showed that job strain was associated with an approximately 20% increased risk of acute ischemic stroke (hazard ratio [HR]=1.24, 95% confidence interval [CI]=1.05–1.47), but not with overall stroke (HR=1.09, 95% CI=0.94–1.26) or hemorrhagic stroke (HR=1.01, 95% CI=0.75–1.36) risk. Using these estimates, Lee and Kim [18] evaluated the job stress-attributable burden of disease in Korea. Approximately 6.9% of strokes were caused by stress at work (4.8% ischemic strokes and 2.1% hemorrhagic strokes). The estimated prevalence of stroke and deaths per 100,000 people were 501 and 59, respectively. In terms of job stress-attributable DALY, the disease burden per 100,000 people was 72.
There has been some debate on whether the effects of “job strain” on stroke are more pronounced when the effects of job demands or controls are assessed independently [16]. Two studies in northern Europe found a relationship between lack of job control and increased risk of stroke [19,20]. These results highlight the importance of job control rather than its interplay with job demands. Regarding gender differences, low job control may predict stroke in women more than in men [21]. In large-scale studies conducted in Sweden, low job control was linked to a higher risk of stroke death in women but not in men, and the risk of intracerebral hemorrhage was higher among women with low job control than among men [19,22]. However, other studies from Japan show that low job control is less helpful for defining CVD risks than combining demand and low control (high-strain jobs) [23].
Ischemic stroke and coronary heart disease share many similar causes, with atherosclerosis being central [17]. Job stress can directly affect the cardiovascular system by activating the neuroendocrine stress response, causing dysregulation of the hypothalamic– pituitary–adrenal axis, or metabolic syndrome. It can also indirectly affect the cardiovascular system by encouraging unhealthy behaviors such as smoking, inactivity, and eating poorly, which are all major risk factors for stroke [24].
Long working hours
Long working hours are well-known risk factors for diabetes and CVD [7] and are closely related to cerebral infarction. Additionally, when working long hours, job stress and sedentary lifestyle increase, which are risk factors for cerebral infarction. From nationally representative matched case-control sets in Korea, the risk of hemorrhagic stroke increased in those with extended duration of working time [25]. A meta-analysis in 2015 also showed a dose-response relationship between long working hours and stroke [26]. Afterward, a WHO/ILO (World Health Organization and the International Labour Organization) Joint Estimate in 2020 confirmed that working ≥55 h/week increased the risk of stroke when followed up between 1 year and 20 years (risk ratio [RR]= 1.35, 95% CI=1.13–1.61; seven studies; 162,644 participants; I2=3%; moderate quality of evidence) [27].
The mechanism by which long working hours cause stroke can be divided into two major pathways [27]. First, long working hours increase unhealthy behaviors, such as smoking, drinking, unhealthy diet, and insufficient physical activity. Sleep disturbances due to long working hours and insufficient recovery time also increase the risk of stroke. Second, long working hours cause chronic psychosocial stress response. The repetitive, high-physical, and psychological effort of long working hours causes an excessive release of stress hormones. Over time, repetitive activation increases stroke risk factors such as hypertension and atherogenesis in the coronary vessels.
According to a case-control study conducted by INTERSTROKE investigators, hypertension contributed to 56% of hemorrhagic stroke cases [4]. Hemorrhagic stroke had a greater correlation with hypertension than ischemic stroke. However, there are conflicting findings regarding long working hours and hypertension [28], and further research is required.
In summary, substantial epidemiological studies have shown that long working hours can be a risk factor for stroke; however, the preventive effect of reducing working hours remains unclear. Stroke prevention consists mostly of medical therapy and lifestyle modification. There have been several reports on the association between working hours and lifestyle [6]; therefore, it would be useful to provide empirical evidence on the effectiveness of this intervention.
Shift work
In “24/7” modern societies, about 20% of the workforce engages in shift work, which plays a significant role in many countries [29]. Shift workers alter their sleep patterns to accommodate unpleasant work schedules, which is contrary to their biological circadian rhythm that is designed for maximum activity during the day and rest at night. Consequently, they endure complicated psychological, physiological, and behavioural stresses [30].
Numerous studies suggest that shift work may have adverse health effects, including cerebrovascular diseases. In a systematic review and meta-analysis by Vyas et al. [31], 34 primary studies recruited 2,011,935 individuals. Shift work status was related to an elevated risk of ischemic stroke using pooled random effects models (RR=1.05, 95% CI=1.01–1.09). Working shifts did not correlate with increased mortality (whether the vascular cause was specific or not). Based on the proportion of shift workers among the adult working population in Canada (32.8%), the population attributable hazards due to shift employment were estimated at 1.6% for ischemic stroke based on data from 2009 and 2010. In another meta-analysis of five studies, shift workers experienced a mildly increased risk of stroke mortality (combined RR=1.03, 95% CI=1.00–1.07) than that of non-shift workers [32]. A recent prospective cohort study of nurses and nursing assistants in Stockholm, Sweden, from 2008 to 2016 comprised 26,667 women and 3,793 men [33]. The findings indicated an increased risk of cerebrovascular disease among employees who worked night shifts more than 30 times (HR=1.44, 95% CI=1.04–1.99), 3 consecutive night shifts more than 15 times (HR=1.69, 95% CI=1.18–2.42), or with more than 30 quick returns (5 years) of exposure to night shift work (HR=1.87, 95% CI=1.27–2.77); all supported by a dose-response pattern. These results demonstrate a relationship between night shift work and increased risk of cerebrovascular disease among nurses and nursing assistants. Stroke risk is increased by working night shifts for an extended period, number of years, working nights consecutively, and taking little time off.
Despite the heterogeneity, possible bias, and inherent methodological weaknesses of the studies, previous findings have provided accumulating evidence supporting the potential relationship between night-shift work and stroke risk. Further experimental and prospective studies with sufficient follow-up are needed to draw clearer conclusions about the causal link between shift work and stroke. These studies should include a comprehensive assessment of shift work, precise definition of stroke, and adjustments for lifestyle, occupation, and sleep characteristics.
Exposure to noise
Noise exposure is a well-known health hazard in workplaces. Noise at work (≥85 dBA) affects approximately 17% of the global labor force [34]. Noise-induced sensorineural hearing loss has long been recognized as the most widespread occupational illness in developed nations [35]. Moreover, the potential extra-aural consequences of noise are recognized for decades in occupational and environmental medicine [36-42]. Heart diseases, such as atherosclerotic coronary heart disease and stroke, are more likely to occur in people who are constantly exposed to noise. Mechanistic evidence have also shown that workplace noise can induce CVDs [43].
Many epidemiological studies have evaluated the relationship between noise exposure and stroke in community and workplace settings. The results of the meta-analysis of nine studies showed a relative stroke risk of 1.013 (95% CI=0.998–1.028) per 10 dB increase in road traffic noise and an estimated 1.3% increase in stroke risk for each additional 10 dB in aircraft noise [44].
Stroke risk due to noise exposure is also evident in workers. In a prospective cohort study, Fujino et al. [45] examined the relationship between male Japanese workers’ perceptions of noise at work and cerebrovascular diseases. The results suggested that perceived noise exposure increased the risk of intracerebral hemorrhage (HR=2.38, 95% CI=1.20–4.7), but did not increase the risk of cerebrovascular diseases, subarachnoid hemorrhage, or cerebral infarction. However, according to WHO/ILO Joint Estimates from two cohort studies of approximately 170,000 participants [46], workers exposed to ≥85 dBA had substantially higher risk of acquiring stroke by 11% (RR=1.11, 95% CI=0.88–1.39) than those without occupational exposure to noise. Increased stroke risk due to noise has been reported, mainly in hemorrhagic than in ischemic stroke [47]. For hemorrhagic stroke, noise is mainly correlated with hypertension and mental stress, which increases the risk of atherosclerotic vascular disease.
Considering the quality of evidence, confidence in effect estimates, and other compelling attributes, evidence remains inadequate for evaluating stroke prevalence, incidence, and mortality. Further studies are required to examine the effect of occupational noise exposure on the prevalence, incidence, and mortality rates of stroke. In the future, researchers should use standardized, high-quality assessments of exposure and outcomes to ensure that evidence is adequate to be compared and harmonized to generate more thorough and quantitative knowledge.
Working in high and cold temperatures
As discussions related to climate change progress, studies on extreme climate environments and cerebrovascular diseases have been conducted [48-50]. Health effects caused by climate likely occur mainly in outdoor workers, such as in construction and agriculture [51,52]. However, several large-scale longitudinal studies on hospitals or population groups in cities have been conducted [53,54]. Recently, literature on the contribution of temperature to disease-induced outcomes when it is higher or lower than the minimum mortality temperature (MMT) has been published [55].
Working in a high-temperature environment is harmful and can lead to health problems including heat exhaustion and heat stroke. A heatwave refers to several days of high temperatures above a certain threshold; although the criteria vary for each study or country, heatwaves contribute to death and hospitalization worldwide. A systematic literature review of heatwave exposure and cerebro-cardiovascular disease published until March 2018 showed that the odds ratio (OR) of morbidity was 0.988 (95% CI=0.960–1.011) and OR of mortality was 1.192 (95% CI=1.042–1.364) [56]. More recent systematic reviews and meta-analyses based on heat exposure (high temperature and heat wave) and cerebro-cardiovascular disease published from January 1, 1990 to March 10, 2022, demonstrated a significant increase in the RR of mortality (1.038, 95% CI=1.031–1.045) due to stroke as temperature increased by 1°C [57]. In contrast, the RR of morbidity was not significant (1.004, 95% CI=0.998–1.010). According to another systematic review and meta-analysis that analyzed only cerebrovascular diseases, the RR of major adverse cerebrovascular events (MACBE), including death (mortality due to stroke), stroke occurrence (morbidity), emergency room visit for stroke (morbidity), and emergency hospital admission (morbidity), increased (RR=1.1%, 95% CI=0.6–1.7) [49]. In other words, when exposed to higher temperatures, stroke mortality rate increases significantly. Moreover, continued exposure for several days, which corresponds to heat waves, further increase ischemic stroke risk.
Working in cold conditions can also be life threatening, causing frostbite, hypothermia, and angina in severe cases. Lian et al. [49] showed a 1.2% (95% CI=0.8–1.6) increase in the RR of MACBE when exposed to low temperatures belonging to the 1st–25th percentiles in the region. Specifically, the RR of hemorrhagic stroke, 1.2% (95% CI= 0.65–1.74) and the RR of ischemic stroke, 0.71% (95% CI=0.40–1.20) increased. According to a case-crossover study comparing 13,201 stroke deaths from November 1981 to April 2015 in Quebec, Canada, the risk of deaths from hemorrhagic stroke at -20°C is reported to be 1.13-fold higher (95% CI=1.1–1.27) compared to the daily minimum temperature of 0°C [58]. Particularly, the OR of hemorrhagic stroke death was 1.17 (95% CI=1.04–1.32) in men, and the OR of hemorrhagic stroke death was 1.12 (95% CI=1.00–1.24) after a 12-h snowfall; however, no significant association was found for ischemic stroke in women. According to a study investigating the relationship between extreme temperatures and mortality rates from 2000– 2013 in Lisbon, the RR of mortality from cerebrovascular disease is 2.09 (95% CI=1.74–2.51) when the temperature falls under 7.3°C (1st percentile of temperatures) based on the MMT of 22°C [59]. However, in studies on workers, there are inconsistent results regarding cold weather and stroke [51]. When working in a low-temperature environment, cold temperatures also seem to increase the risk of morbidity and mortality of cerebrovascular disease, and the risk increases as the extreme temperature decreases. However, this has not been confirmed by research on workers.
Many studies on high and low temperatures and the risk of cerebrovascular disease have reported a nonlinear U-, V-, or J-shaped correlation based on MMT (approximately 25th–75th percentile of the annual range of temperatures in a particular region) [49]. When placed in a hot environment, sweating and skin blood flow induce dehydration, which can increase blood viscosity and the risk of ischemic stroke. Cold environments stimulate sympathetic nervous systems, which increase blood pressure, constrict peripheral blood vessels, and increase platelet levels which increases the risk of cerebrovascular disease [60]. Cold stress itself theoretically increases the brain’s oxygen demand, which can increase brain blood flow and worsen brain ischemia. When exposed to a hot environment, blood vessels expand through thermoregulatory mechanisms. These eventually decrease blood flow to the brain due to increased heart rate and sweating, which can devastate the existing ischemia [61].
In summary, considering the results of large-scale epidemiological studies and physiological mechanisms, working at high and cold temperatures affects mortality owing to the incidence and deterioration of cerebrovascular diseases. Temperature affects various cerebrovascular diseases. Due to the characteristics of climate research, studies on the delay effect and climate adaptation by region are required. Additionally, more studies should deal with working population that are directly affected by ambient and extreme temperatures compared with the general population. Other climate factors, such as diurnal temperature changes [52,54] and sensible temperatures, including humidity and wind speeds, should be investigated further.
Exposure to dust (air pollutants)
Air pollutants are a relatively recently identified risk factor for stroke. Unlike traditional risk factors, pollutants can explain the global variation in stroke distribution and short-term risk factors that trigger increased stroke events in a particular period [62]. The major air pollutants are particulate matter (PM2.5, PM10), ozone (O3), sulfur dioxide (SO2), nitrogen oxides (NOx), and carbon monoxide (CO). These are emitted from fossil fuels, transportation, and industry. Although the relationship between air pollutants and stroke has been extensively studied, research on occupational exposure to stroke remains lacking. Occupations reported as being exposed to dust with an increased CVD risk include miners, agricultural workers, and chimney sweepers [63].
The mechanism for ambient pollution leading to stroke involves the translocation of nanoparticles, inflammation, and lipid modification related to oxidative stress and autonomic dysfunction [62]. Nanoparticles enter the systemic circulation through the lungs and cause systemic inflammation and atherosclerosis. Pathways mediated by inflammatory and reactive oxygen species promote coagulation, endothelial dysfunction, atherogenesis, metabolic disorders, and hypertension. Inhaled pollutants are associated with adverse effects on heart rate variability, which is a marker of cardiac autonomic dysfunction and a predictor of arrhythmia [64], which is a key risk factor for stroke due to embolisms and small vessel occlusions.
To the best of our knowledge, stroke is considered to be related to air pollutants, although results have been inconsistent. Rojas-Rueda et al. [65] reported that a significant relationship was confirmed by moderate evidence (HR=1.11, 95% CI=1.05–1.17) for the long-term effects of PM2.5 and low evidence (RR=1.15, 95% CI=1.06–1.24) for the long-term effects of environmental tobacco smoke. In a recent case-crossover study of 412,567 stroke deaths in China, a 10 μg/m3 short-term increase in PM2.5, PM10, SO2, NO2, CO, and O3 levels was associated with 1.44%, 0.93%, 5.55%, 2.90%, 0.148%, and 0.54% increase in the odds of mortality from ischemic stroke, respectively [66]. In contrast, research using a large cohort of stroke patients in the US, the REGARDS (REasons for Geographic and Racial Differences in Stroke) cohort, found no association with PM2.5 [67]. The possibility of misclassification of exposure was presented because of the use of population addresses.
However, studies of occupational exposure to ambient pollution and its impact on stroke are scarce. For 176,309 Swedish male construction workers occupationally exposed to inorganic dust, wood dust, fumes, gases, and irritants and 71,778 unexposed, exposure significantly increased the risk for ischemic heart disease (RR=1.13, 95% CI=1.07–1.19), but not for cerebrovascular disease (RR=0.97, 95% CI=0.88–1.19). The researchers mentioned that the control group was also exposed to air pollutants to some degree [68]. In a recent study, low-density lipoprotein and homocysteine levels were measured as CVD biomarkers in 65 Swedish workers. With a higher exposure intensity or a longer year of exposure to air pollutants, homocysteine levels were higher [63].
In summary, although the epidemiological study results are limited, ambient pollutant exposure may be related to stroke. The nature of ubiquitous exposure makes it possible to report the numerically reduced effects. Moreover, many studies have been conducted in Europe and the US, whereas air pollutant levels tend to be higher in developing countries [62]. Therefore, underestimating the true risk should be considered when interpreting the results. The exposure levels of gig workers, such as delivery service and traditional outdoor workers, should be further investigated to protect them from the adverse health effects of ambient pollution in future working environments.
Chemical exposures
Exposure to several chemicals, such as lead (Pb), arsenic (As), mercury (Hg), cadmium (Cd), and CS2, is a potential risk factor for stroke [69]. However, only a few epidemiological studies have reported an association between occupational chemical exposure and cerebrovascular disease [70]. Chemical exposure is more common in developing countries. Recent studies have explained the increased risk of cerebrovascular disease at low levels of chronic environmental exposure, which induces a more serious burden in developing countries [71]. As such, chemical exposure is worthy of attention in stroke prevention.
Mechanism
Chemical exposure contributes to cerebrovascular diseases through various mechanisms. It increases intracranial carotid atherosclerosis by increasing radical production, oxidative stress, thrombotic risk, and promoting vascular inflammation [72,73]. Exposure damages the endothelium of the cerebral blood vessels, causing microvascular dysfunction and altering cerebral blood flow, thereby increasing the risk of stroke [74]. Additionally, many epidemiological studies have found a relationship between heavy metal exposure and high blood pressure [28], which is one of the strongest risk factors for cerebrovascular disease.
Lead
Pb exposure is a diverse process that includes battery, steel, dye, and pigment manufacturing processes. Pb compounds are also widely distributed in gasoline, paint, air, and soil [75]. In a study using data from the National Health and Nutrition Examination Survey (NHANES) in Korea, when analyzed among hypertensive patients, the group with high blood Pb concentration reported a stroke OR of 2.36 (95% CI=1.02–5.54) [76] compared to the group with low blood Pb level. Using data from the NHANES II mortality follow-up study in the US, from 1976 through 1992, Lustberg and Silbergeld [77] identified that blood Pb levels of 20–29 μg/dL (1.0–1.4 μmol/L) had a 39% increase in circulatory mortality (RR=1.39, 95% CI=1.01–1.91, including cerebro-cardiovascular disease), than those with blood Pb levels <10 μg/dL (<0.5 μmol/L). However, inconsistent results were found in the worker cohort. In a cohort study of Pb-exposed smelter workers, the standardized mortality ratio for cerebrovascular disease was 129 (P<0.01); however, this association was not significant when limited to the long-term exposure group. There may have been an uncontrolled selection bias; therefore, caution should be exercised.
Mercury
Hg is a heavy metal that poses serious health hazards to humans. About 44.75 million people in 80 countries work in artisanal and small-scale gold mining [78]. This results in serious exposure to Hg through both environmental and occupational processes. Hg is linked to several vascular disorders, including blood-brain barrier damage, endothelial dysfunction, and stroke [72]. Meanwhile, in a recent meta-analysis of 14 studies regarding the mortality of each disease, coronary vascular disease was related to Hg exposure; however, Hg exposure and stroke were not significant [79]. In the REGARDS cohort data, no association was observed between serum Hg concentration and incidence of ischemic stroke (the highest vs. lowest quintile of Hg levels: HR=0.82; 95% CI=0.55–1.22; P for linear trend=0.42) [80].
Arsenic
Inhaling metal particles and drinking water are the major causes of chronic As exposure [81]. As is used in some paints, wood preservatives, agricultural chemicals, and glass manufacturing [82]. Wang et al. [83] reported a dose-response association in the increase in carotid atherosclerosis with chronic exposure to inorganic As. However, epidemiological data are inconsistent. As exposure was associated with CVD but not stroke in a meta-analysis of 31 studies (8 on stroke prevalence/mortality) [84]. Using the REGARDS data, Tsinovoi et al. [85] found no association between total As and inorganic As. MMA, a metabolite of arsenic, is positively associated with ischaemic stroke; however, MMA can also be derived from sources other than As.
Cadmium
Cd is a naturally occurring heavy metal used in batteries, electronics (such as TV screens and lasers), and beauty products. Evidence indicates that Cd can induce brain vascular pathology in the context of small vessel disease and atherosclerosis [74]. Using the REAGRDS data, Chen et al. [86] observed that urinary Cd was associated with an increased incidence of ischemic stroke (quintile 5 HR=1.50 [reference; quintile 1], 95% CI=1.01–2.22, P for trend=0.02). However, the result was not significant among nonsmokers (tertile 3 vs. tertile 1: non-smokers: HR=1.27, 95% CI= 0.80–2.03, P for trend=0.29; smokers: HR=1.60, 95% CI=1.06–2.43, P for trend=0.07, P for interaction=0.51).
Carbon disulfide
The association between CS2 and cerebrovascular disease has mainly been studied in viscose rayon plants in CS2-exposed workers. Moreover, epidemiological evidence has been reported regarding cerebrovascular disease. Liss and Finkelstein [87] reported more deaths than expected from cerebrovascular disease in a population that worked at the viscose rayon plant in Ontario. Mortality due to stroke was higher than expected (proportional mortality ratio=207, P<0.05; reference: general population of Ontario). The risk of stroke in the high-exposure subgroup was significantly increased compared with other workers in the same plant (OR=4.92, 95% CI=1.66–14.65). In Korea, retired workers from a rayon manufacturer reported that 52.1% of workers among the 117 ex-employees from the rayon plant, W company, had cerebral infarction [88]. In a 2004 cohort study of Japanese viscose rayon factories, exposure to CS2 under the current Japanese occupational exposure level, 10 ppm, might have increased the number of high-signal intensities, which presented as so-called “silent cerebral infarctions” in brain magnetic resonance imaging. Final OR for the exposed was 2.27 (95% CI=1.37–3.76) [89].
Summary
In summary, a considerable mechanistic basis was identified for the association between chemical exposure and cerebrovascular disease; however, the epidemiological report was relatively weak. Some of these limitations indicate an unknown bias in occupational settings. Moreover, many chemicals have adverse effects on the general population via environmental routes and their occupational effects may be numerically attenuated.
Conclusion
Substantial research has been conducted on the influence of occupational factors on stroke. The results of this review suggest that there is sufficient evidence to support the relationship between increased risk of stroke and job stress, working in extreme temperatures, long working hours, and/or shift work. The association between stroke and occupational exposure to noise or chemicals remains inconclusive, although several studies have reported this finding. Additionally, various other occupational factors have been documented to be related to stroke: for example occupational physical burden [90]. However, these factors were not covered in this review, because only fragmentary evidence exists for this.
Recently, the WHO proposed a new global indicator for worker health based on mortality rate from diseases attributable to selected occupational risk factors [91]. The total estimated number of deaths attributable to occupational risk factors increased by nearly 40% in 2016 (744,924 out of 1,879,890 deaths) after adding two new exposure-disease pairings (deaths from stroke or ischemic heart disease attributable to long working hours) [92]. Other exposure-disease pairs should be considered in the comparative risk assessment if there is adequate evidence to justify this. The results of our review suggest that strokes caused by job stress, working in extreme temperatures, and/or shift work could be candidates for further exposure-disease pairings.
Further occupational risk factor research should address the following questions to provide better evidence. Stroke is most common in the elderly and is a disease of retirement age, which means that unless the research is prospective with long-term follow-up, the true impact might be overlooked if a study only investigates short-term associations. Moreover, although difficult to separate, socioeconomic factors such as income, education, and employment should be recognized as key factors in stroke. Therefore, it is highly recommended that future research use a life-course approach to investigate how people’s professional lives grow over the course of their lifetime while considering the socioeconomic context.
This review has important clinical and public-health implications. From a clinical perspective, assessing occupational factors can help identify at-risk workers. Accordingly, increasing clinical knowledge of the health impacts of occupational factors may enhance the prevention and management of stroke at both individual and community levels. From a public health standpoint, reducing exposure to occupational risk factors should be the main goal of workplace programs and health policies for the primary prevention of stroke.
Notes
Funding statement
None
Conflicts of interest
The authors have no financial conflicts of interest.
Author contribution
Conceptualization: MYK. Study design: MYK. Methodology: MYK. Data collection: MY, HY, SYK, OK, MWN. Investigation: MY, HY, SYK, OK, MWN. Writing—original draft: MY, HY, SYK, OK, MWN, MYK. Writing—review & editing: MY, KWP, MYK. Approval of final manuscript: all authors.