Introduction
Stroke is a major cause of hospitalization and adverse long-term consequences globally.1,2,3 Notable among the consequences of stroke is poststroke fatigue (PSF) especially because of its prevalence, persistence and adverse impact on outcomes across the stroke trajectory.4,5 Hence, PSF, often described in terms of extreme and persistent tiredness, weakness or exhaustion which is not traceable to previous experiences of exhaustion,6 is increasingly gaining prominence in stroke research and care.4
On the subject of its prevalence, PSF has been reported to affect a third of all stroke survivors7 while prevalence rates as high as 73% have also been reported.4 Studies have also shown that PSF may persist for several years after a stroke event.8,9,10,11 For instance, reports from a nationwide study in Sweden showed that up to 39% of stroke survivors still experienced PSF 2 years after stroke.8 Regarding the impact of PSF, increased mortality and poor rehabilitation outcomes have been reported.8,10,12 Such poor rehabilitation outcomes include delayed functional recovery or persistent functional deficits,10 institutionalization8 and diminished health-related quality of life (HRQL).5,9,10,13
Identifying the association between PSF and HRQL in stroke survivors is of particular importance. As a multidimensional construct, HRQL is central to human existence and its enhancement can be regarded as the ultimate goal of rehabilitation following a life changing disease such as stroke.14,15 Therefore, identifying the association between PSF, a modifiable poststroke sequla, and HRQL may assist in enhancing HRQL of stroke survivors. Efforts at identifying the impact of PSF on poststroke HRQL have however not received the required global attention with no apparent contribution from African countries. This dearth has persisted despite the increasing number of studies on poststroke HRQL from the African continent in recent times,16,17,18,19,20,21,22 especially from Nigeria.16,18,19,22 With most of the data on PSF and HRQL emanating from Western5,9,10 and Asian13 countries where cultural, socio-economic and healthcare systems are diverse from what obtains in Africa, the need for country- or continent-specific information comes to the fore. For instance in terms of healthcare, health insurance is a very recent development in many African countries such as Nigeria and health expenditures are still borne directly by the majority of the population unlike what obtains in industrialized countries. Similarly, health services in terms of health facilities and personnel, especially in the field of rehabilitation, are not as robust as those of developed countries. In order to provide the required setting-specific data therefore, this study sought to identify the impact of PSF on global and domain-specific HRQL of stroke survivors in Nigeria, the most populous country in Africa.
Methods
Study design
This cross-sectional study was approved by an Institutional Research and Ethics Committee in Nigeria.
Participants
One hundred out of the 129 stroke survivors receiving oupatient physiotherapy at two tertiary hospitals in Northern Nigeria were recruited during a 3-month period. Eligibility criteria included being at least 18 years of age, willingness to participate in the study by provision of informed consent, ability to sufficiently communicate verbally to have the study instruments administered, and absence of co-morbid conditions that may result in fatigue (e.g., rheumatoid arthritis and cancers). All the stroke survivors though community-dwelling, were recruited and assessed at the physiotherapy clinics of the 2 tertiary hospitals where they were receiving poststroke physiotherapy care on outpatient basis. Typically in Nigeria, post-acute stroke rehabilitation predominantly involves outpatient physiotherapy due to the unavailability of inpatient or community-based rehabilitation facilities and also because of the scarcity of other rehabilitation professionals.
Instruments
Data Form
Socio-demographic and clinical data were obtained using the data forms specifically designed for that purpose. Information obtained included gender, age, marital, pre-stroke employment and educational status, stroke sub-type, nature of stroke (first-ever or recurrent), side of stroke and time of stroke onset. Information on socio-demographics were obtained from the stroke survivors while clinical data were obtained and/or confirmed from the hospital clinical notes of each stroke survivor.
Fatigue Severity Scale (FSS)
The nine-item FSS23 was used to assess PSF in the stroke survivors. The items are scored on a 7-point Likert scale that ranges from 1 (strongly disagree) to 7 (strongly agree). The total score on the scale is the arithmetic mean of the total score obtained from the nine items. Total score ranges from 1 to 7 and higher score depicts higher impact of fatigue on daily activities. The FSS has an excellent internal consistency (Cronbach's α = 0.88) and is the most commonly used scale for assessment of PSF.4
Health-Related Quality of Life in Stroke Patients-26 (HRQOLISP-26)
The HRQOLISP-26 is a stroke-specific quality of life measure. With 26 items in 4 domains namely physical, emotional, cognitive and eco-social, each domain score was obtained by simple summation and transformation into a scale of 100 while overall HRQL score was generated by finding the arithmetic mean of the domain scores. Higher domain and overall scores depict better quality of life and the highest obtainable score is 100. The HRQOLISP-26 has good construct and criterion-related validity. The scale also has good test-retest reliability and internal consistency in Nigerian stroke survivors (Cronbach's α=0.89).24
Modified Rankin Scale (mRS)
The mRS was used to assess the functional status of the stroke survivors. The mRS is a widely used scale in stroke studies and the 5-level version that assess disability on a scale of 0 (no disability) to 5 (severe disability) was used. The mRS is a brief and reliable measure of level of global functional independence in individuals with stroke.25
Procedure
Following the provision of written informed consent, socio-demographic, clinical, poststroke fatigue, and HRQL data were obtained from the stroke survivors using the aforementioned instruments through face-to-face interviews. Interviews were conducted prior to physiotherapy sessions and spanned approximately 20 minutes for each stroke survivor. All data were collected by the second author from February to April 2013.
Statistical analyses
Socio-demographic, clinical, PSF and HRQL data were summarized using descriptive statistics of frequencies, percentages, mean and standard deviation as appropriate.
Spearman rank order correlation analyses were used to assess the bivariate associations between PSF and HRQL (overall HRQL and domains). Univariate (Mann Whitney U and Kruskal Wallis tests for categorical variables) and Spearman rank order correlation (for continuous variables) analyses were also conducted to identify the associations between HRQL and socio-demographic (age, gender, education, pre-stroke employment, marital status) and clinical (stroke sub-type, laterality, nature of stroke, functional status, and poststroke duration) attributes. These analyses were carried out for each of the four HRQL domains and overall HRQL and those socio-demographic and clinical variables that were found to be significantly associated with overall and domain-specific HRQL were controlled for in the multivariate analyses.
Using the hierarchical regression analyses, we examined the independent impact of PSF on the domains and overall HRQL. All the socio-demographic and clinical variables that emerged significant in the univariate and bivariate analyses were entered into the first step (step 1) of the hierarchical regression analyses while PSF was the sole variable introduced in the second step (step 2). This process was repeated for each of the 4 HRQL domains and overall HRQL, they being the dependent variable. Level of statistical significance was set at 0.05.
Results
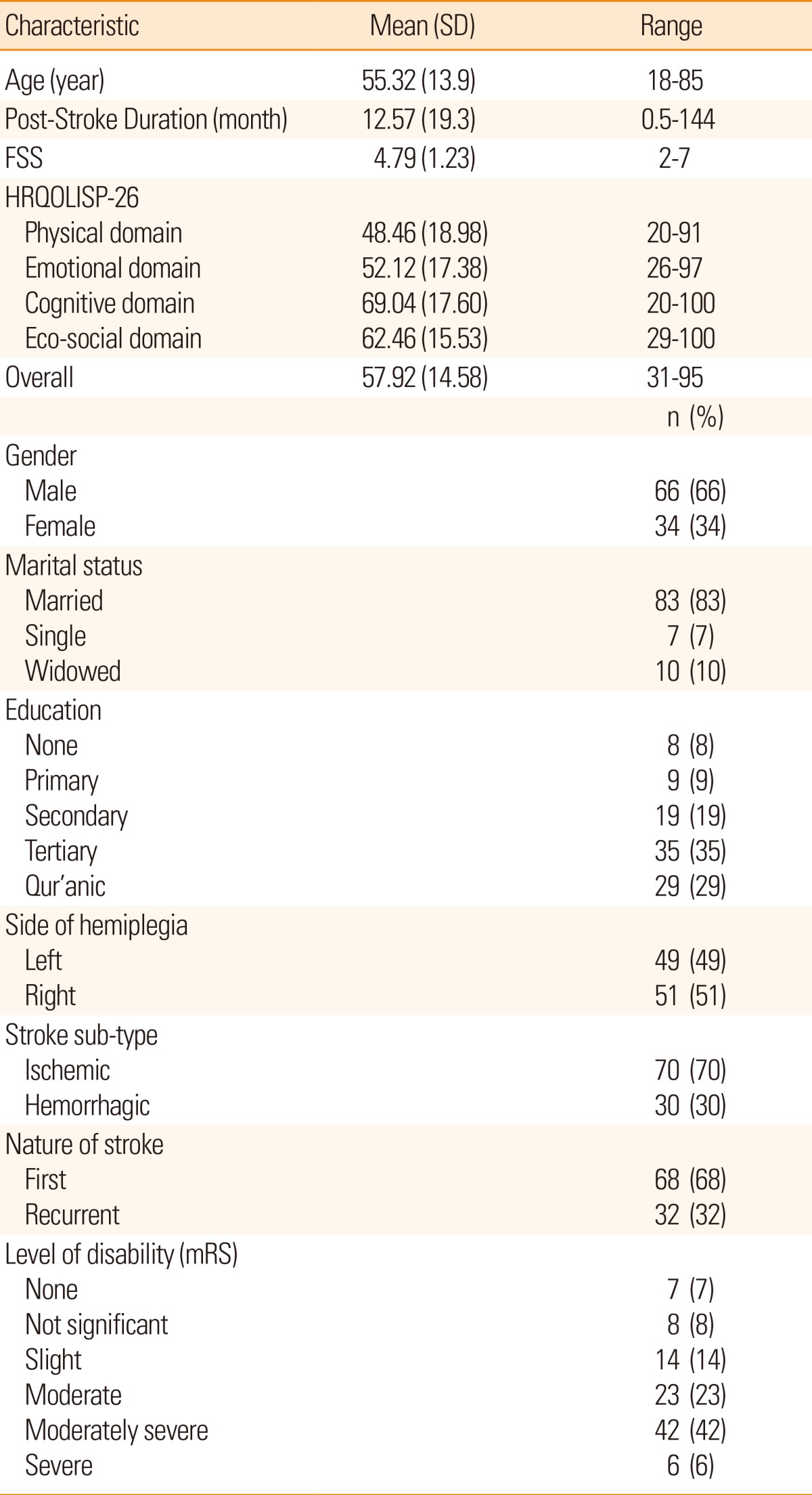
One hundred stroke survivors with a mean age of 55.3 (SD 13.9 years) (range 18-85 years) and who had suffered stroke for an average of 12.6 months (SD 19.3 months) participated in the study. The majority were males (66%), married (83%), had suffered ischemic stroke (70%) and presented with moderately severe disability (42%). Mean overall HRQL score was 57.92 (SD 14.58) while mean FSS score was 4.79 (SD 1.23) (Table 1). Table 1 also shows the mean scores of the HRQL domains with the highest and lowest scores recorded in the cognitive and physical domains respectively. The stroke survivors were recruited from 2 tertiary hospitals and there were no differences in their socio-demographic, clinical, PSF and HRQL data.
Univariate and bivariate analyses
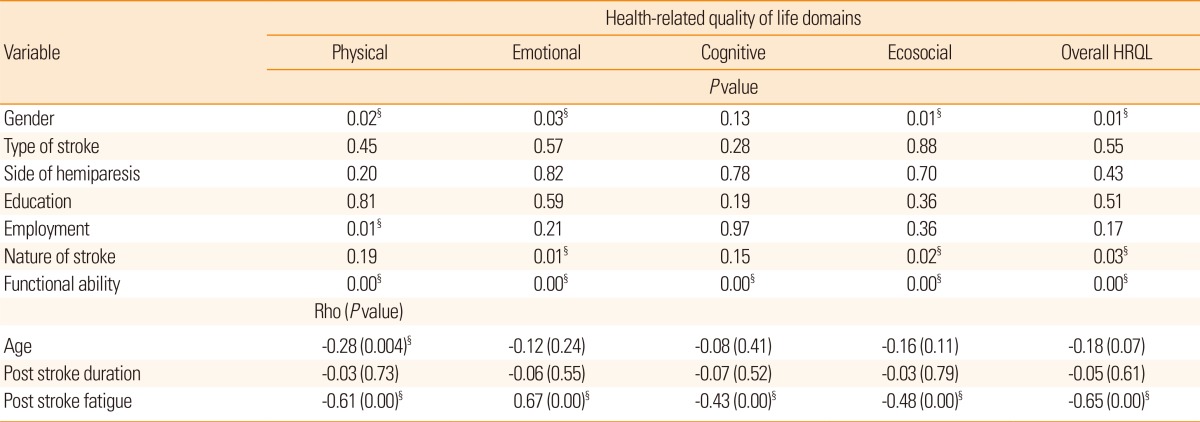
Spearman correlation analyses between FSS and HRQL overall and domains were significant at P<0.0001. Correlation coefficients for associations between overall, physical, emotional, cognitive and ecosocial domains of HRQOLISP-26 and FSS were -0.65, -0.61, -0.67, -0.43, and -0.48 respectively. Correlation analyses between HRQL and continuous socio-demographic and clinical variables, namely age and poststroke duration, did not yield statistically significant results except for the negative correlation between age and physical domain of HRQL at P<0.01 (Table 2).
Results of Mann Whitney U and Kruskal Wallis tests for associations between HRQL and categorical socio-demographic and clinical factors are presented in Table 2. The table shows that of all the categorical variables, only functional status was significantly associated with all the HRQL domains and overall HRQL (P<0.0001). In addition to this, other significant variables were gender and pre-stroke employment for the physical domain. For each of ecosocial HRQL and overall HRQL, the significant variables were gender and nature of stroke while for emotional HRQL, gender, marital status, and nature of stroke were significant. These socio-demographic and clinical variables that emerged significant in the univariate and bivariate analyses were entered into step 1 of the hierarchical regression analyses for the respective HRQL domains.
Multivariate analyses
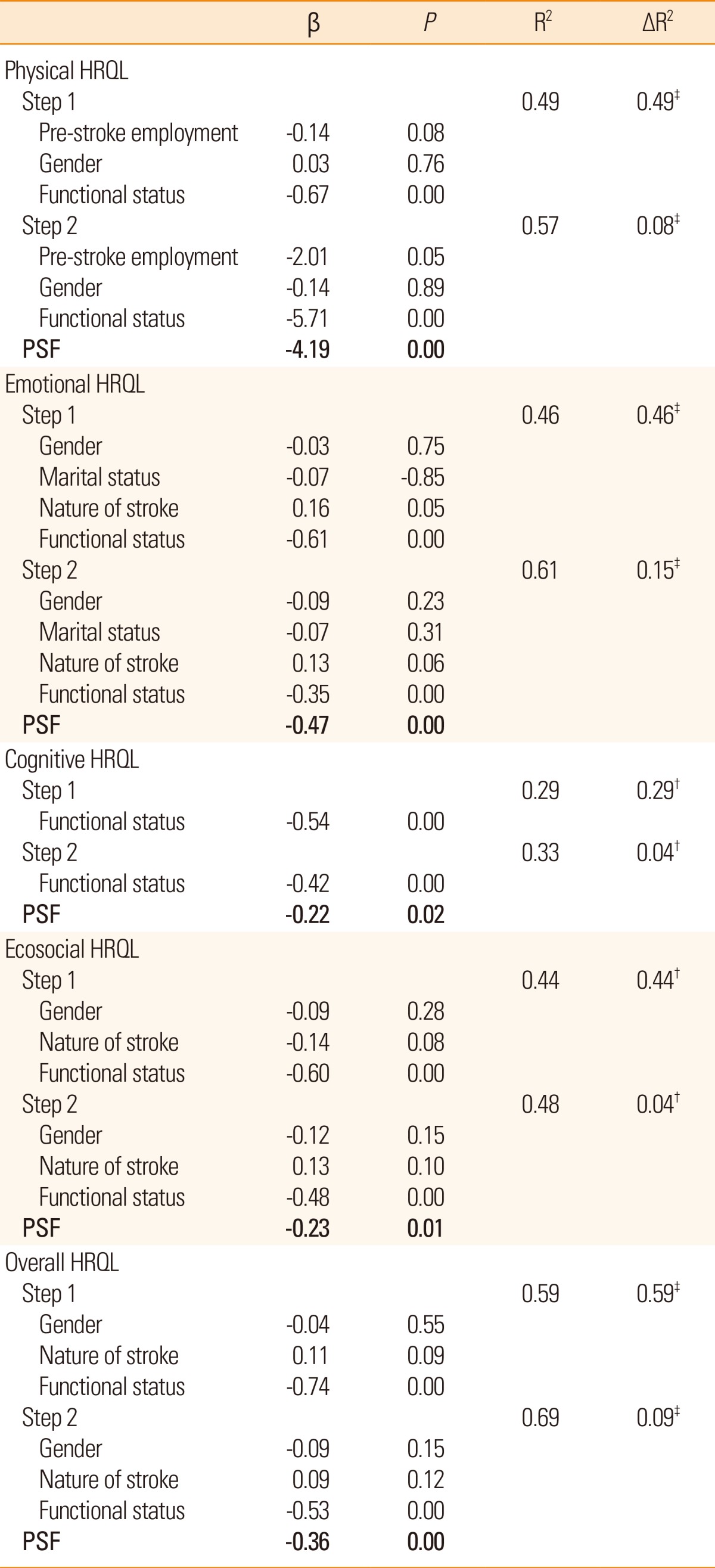
Table 3 shows the results of the hierarchical regression analyses. Five hierarchical regression analyses were conducted for each of the four HRQL domains and overall HRQL (dependent variables). As mentioned above, step 1 of each regression analysis included socio-demographic and clinical variables that emerged significant in the respective univariate and bivariate analyses. This was done in order to control for the effect of those variables on HRQL before assessing the independent impact of PSF on HRQL. For the physical domain of HRQL, the variables controlled for were age, gender, pre-stroke employment and functional status while gender, nature of stroke and functional status were controlled for in each of the analyses for ecosocial HRQL and overall HRQL. For emotional HRQL, gender, marital status, nature of stroke and functional status were controlled for while functional status was the only variable that was significantly associated with cognitive domain of HRQL in the univariate analysis and was subsequently controlled for in the regression analysis for the domain.
After controlling for the socio-demographic and clinical attributes that were found to be significantly associated with HRQL as outlined above, PSF, which was the only variable entered into step 2 of the regression analyses, was found to have statistically significant association with overall and all 4 domains of the HRQL albeit at varying degrees (Table 3). The greatest impact of PSF was observed in the emotional domain with PSF solely accounting for 15% (ΔR2=0.15) of the variance in that domain at P<0.0001 while PSF contributed only 4% (ΔR2=0.04) to the variances in the cognitive and ecosocial domains at P<0.05 respectively (Table 3). In addition to PSF however, functional status as assessed with the Modified Rankin Scale was also found to be significantly associated with HRQL in all the regression models (Table 3). The observed significant influence of both PSF and functional status on HRQL prompted us to investigate the association between functional status and PSF using one-way ANOVA; we found a statistically significant association (F =8.40; P<0.0001) with higher levels of functional ability related to lower levels of PSF.
Discussion
Poststroke fatigue is an often neglected but important stroke sequela with far reaching consequences.4,26 This study examined the impact of PSF on the HRQL of a group of individuals who had survived stroke in Nigeria, which to our knowledge may assist in bridging the hitherto existing gap in the stroke literature.
Our results showed that PSF was significantly associated with all aspects of HRQL in both bivariate and multivariate analyses with higher levels of PSF associated with lower HRQL. Aside from functional status which appeared to mediate the influence of PSF on HRQL, the influence of PSF subsisted irrespective of the stroke survivor's marital status, gender, age, pre-stroke employment, or whether stroke was recurrent or first-ever. This apparent sweeping influence of PSF on all the dimensions of HRQL was reported in a previous study of Chinese stroke survivors.13 A report from Norway equally showed a near complete influence of PSF on HRQL with only the HRQL domain on emotional role functioning exempt from the influence.9 On the one hand, the seeming all-encompassing influence of PSF may be due to its multidimensional structure, comprising physical, emotional and cognitive components,27 a structure that is observable in the Fatigue Severity Scale23,28 used in our study and the above cited studies. These observations may on the other hand be indicative of a truly profound impact of PSF on virtually all aspects of HRQL poststroke irrespective of settings, which implies that addressing PSF may go a long way in enhancing stroke survivors' HRQL.
It is important to note that the level of association between PSF and the domains of HRQL in this present study varied, with the highest level of correlation observed between PSF and emotional HRQL and the lowest correlation between PSF and cognitive and ecosocial HRQL. The comparatively higher impact of PSF on the emotional domain of HRQL is in line with existing reports5,13 and implies that PSF is a strong determinant of emotional well-being after stroke. Hence, therapeutic efforts aimed at optimizing poststroke emotional well-being may be more effective when PSF is addressed. The existence of a close and bi-directional link between PSF and emotional status of stroke survivors has also been severally reported with some submissions describing PSF as more of a psychological construct than a physical one4,7,12,29,30,31 and suggesting that addressing PSF may be required for enhancing poststroke emotional status and vice versa. It is therefore not surprising that some of the few treatment protocols available for the management of PSF have emphasized neuropsychological and behavioral therapies.6,32
As observed in this study, physical HRQL represents one of the most severely affected HRQL domains after stroke probably because of the motor impairments and functional limitations that accompany the disease.9,15 Hence, identifying determinants of poststroke physical HRQL is particularly important in order to device effective means of enhancing the domain. The impact of PSF on the physical domain of HRQL in this study was pronounced, coming after its impact on emotional HRQL. Contrary to this observed pattern, a longitudinal study found a stronger association between PSF and physical wellbeing than between PSF and mental well being5 while one cross-sectional study observed the weakest association between PSF and physical wellbeing.13 In another cross-sectional study, the strength of the relationship between PSF and physical HRQL ranked 4th out of the 8 HRQL domains assessed.9 Although the reasons for these variations especially regarding the impact of PSF on physical HRQL appear to be unclear, the differences in the HRQL assessment tools used in the different studies could be contributory. However, going by the fact that PSF implies physical or mental exhaustion,33 the strong relationships between PSF and the emotional and physical HRQL observed in our study are justified.
Compared to the other domains of HRQL, the cognitive and eco-social domains had weak (though significant) associations with PSF. Also worthy of note is the highest mean score (69 out of 100) recorded in the cognitive domain which is indicative of better HRQL status compared to the lower mean HRQL scores in the physical (48.4 out of 100) and emotional (52 out of 100) domains. These findings imply that cognitive HRQL of the stroke survivors in this study was relatively spared and was not as dependent on PSF as the other HRQL domains; although the relatively better cognitive status may be due to the inclusion of only stroke survivors with sufficient cognitive ability required to respond to the study's assessment tools. However, while our study examined the impact of PSF on cognitive HRQL, there are also reports on the influence of cognitive status in the development of PSF34 and the importance of cognitive training in the prevention and management of PSF,6 which indicate the bi-directional relationship between the two constructs.
In addition to the impact of PSF on HRQL, we observed that functional status also exerted significant influence on all the domains of HRQL in the multivariate regression analyses implying that functional status and PSF both emerged as determinants of overall and domain-specific HRQL. This finding suggests that functional status could have been influenced by PSF and had possibly mediated the relationship between PSF and HRQL, an assumption supported by a previous report on the adverse impact of PSF on poststroke functional status.10 It may therefore follow that the negative impact of PSF on functional status resulted in diminished HRQL. This is as previous studies have shown functional status as a major determinant of HRQL.9,15 To explore the possible mediating role of functional status in the relationship between PSF and HRQL, we assessed the relationship between PSF and functional status and found a significant association between the two constructs with higher levels of PSF among stroke survivors with lower functional status. In clinical practice, a likely scenario regarding the effect of PSF on functional status and the mediating role of functional status in the relationship between PSF and HRQL could be that PSF adversely affects rehabilitation participation and compliance, with a consequent adverse effect on functional ability (an important rehabilitation focus and outcome) which in turn impairs HRQL. Therefore, going by the significant influence of PSF on an important and holistic construct such as HRQL coupled with the widely acknowledged neglect of PSF both in stroke research and care, the need for routine assessment and screening of stroke survivors for PSF and the urgent requirement for proven and cost-effective therapies capable of improving PSF are emphasized.
This study has a number of limitations. Its hospital-based design may have resulted in selection bias and limited the generalizability of findings. Similarly, the small size of the sample of stroke survivors that participated in the study may limit generalization. The fact that we did not assess depression in this study also constitutes a limitation due to its close association with PSF and HRQL, and the indications that depression may moderate the relationship between PSF and HRQL.10 Reverse causality in the association between PSF and HRQL can also not be ruled out due to the cross-sectional design of the study and this could be addressed in future studies with longitudinal designs.
Conclusion
The outcome of this study showed that in spite of the multidimensional nature of HRQL, PSF had a significant impact on the HRQL construct in its entirety (as assessed in this study), even after accounting for the influence of several socio-demographic and clinical factors on HRQL. Our findings appear to emphasize the need to adequately and appropriately address PSF in poststroke rehabilitation strategies in order to enhance stroke survivors' HRQL especially as PSF is potentially modifiable and treatable.