Acute Ischemic Stroke in Nonconvulsive Status Epilepticus–Underestimated? Results from an Eight-Year Cohort Study
Article information
Dear Sir:
Acute ischemic stroke (AIS) can be associated with status epilepticus (SE). Among 889 patients hospitalized for AIS and prospectively monitored with continuous electronecephalography (EEG)-monitoring, nonconvulsive SE (NCSE) was detected in 3.6% [1]. This finding suggests that AIS may cause NCSE and may prompt clinicians to look for AIS in patients hospitalized for SE of yet unknown etiology. However, the frequency of AIS among patients hospitalized for SE is unknown. In the present observational study, we assessed the frequency of AIS in a cohort of consecutive patients hospitalized in an intensive care unit (ICU) for EEG-confirmed SE.
From January 2005 to December 2012, all SE patients ≥18 years of age admitted to the ICUs of the University Hospital Basel, Switzerland, were consecutively enrolled in a prospective database. All patients underwent at least one EEG >30 minutes or continuous video EEG-monitoring, uncovering SE from different etiologies. SE was defined according to the current guidelines for the evaluation and management of SE [2,3]. Patients with SE following hypoxic encephalopathy were excluded from this study. We identified all patients who had AIS as confirmed by diffusion weighted and apparent diffusion coefficient magnetic resonance imaging (MRI) within ±7 days from onset of SE.
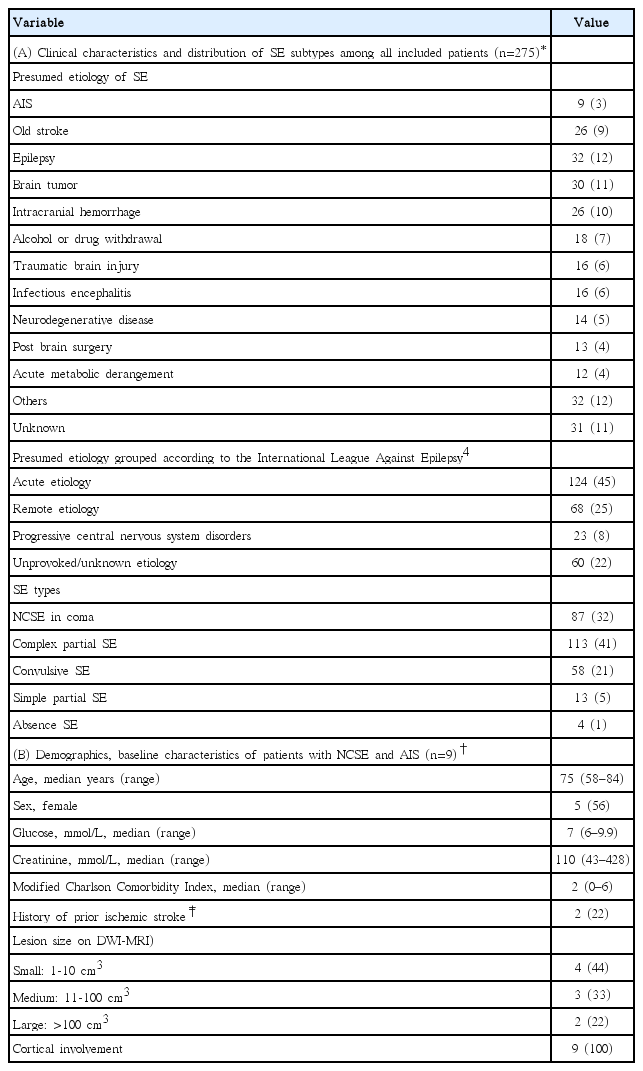
Of 333 consecutive patients with SE enrolled in the SE database, 275 patients were included in the present analysis, 58 patients with hypoxic encephalopathy were excluded. The distribution of different types of SE is shown in Table 1; four out of five patients had NCSE. Table 1 displays the proportion of presumed etiologies of SE within the cohort. An acute etiology according to the International League Against Epilepsy [4] was found in 124 patients (45%). Overall, of 275 patients with SE, 262 (95%) had any cerebral imaging (MRI, computed tomography [CT], or both) within ±7 days from SE onset. Brain MRI was performed in 128 SE patients (49%, 128 of 262), the remaining 134 patients had CT only.
Brain MRI identified AIS in nine patients, i.e. in 7% of all patients undergoing MRI and 3% of the whole cohort. AIS accounted for 7.2% of all patients with an acute etiology (according to the International League Against Epilepsy) [4] underlying SE. Chronic stroke was identified as underlying etiology of SE in 26 patients (9%). AIS involved both the cortex and white matter in all patients, with an ischemic pattern implying primary AIS rather than an ischemic injury secondary to sustained seizures. Among nine patients with AIS confirmed by brain MRI, three patients had no CT-signs of early or chronic brain ischemia. In patients with a CT negative for ischemia, MRI was performed within a median of six days (range 3-7 days) after the diagnosis of SE. All patients with AIS had NCSE, and other plausible etiologies of NCSE were not identified. Four AIS-patients (44% of AIS-patients) died after a median of 20 hospitalization days (interquartile range 12.3-48 days).
The three key findings of this study are: (1) a 7% AIS-frequency in patients hospitalized for SE undergoing MRI; (2) one third of patients with AIS were missed on cerebral CT; (3) the ischemic pattern on brain MRI and the lack of other NCSE-etiologies suggests that the AIS itself may have triggered NCSE.
Previous studies identified acute cerebrovascular disease in 8–22% of patients to be the underlying etiology of SE [5-7]. Although in line with these previous studies, the rather small number of AIS in our SE cohort might result from our strict criteria of close temporal association of AIS and SE (i.e. 7 days), a definition which is missing in the aforementioned studies.
Recently, Algethamy et al. [8] underscored the added value of brain MRI over cerebral CT in ICU-patients with neurological impairment. Among ICU-patients undergoing both a brain CT and MRI, in 95% “MRI revealed clinically relevant additional abnormalities over CT”. The added sensitivity of brain MRI over cerebral CT was greater in the detection of ischemic stroke and neoplastic lesions [8]. In another study on ICU-patients who underwent brain MRI for neurological impairment, AIS was uncovered in 40% (59/146), along with a high burden of white matter hyperintensities. Notably, patient transport from the ICUs to the MRI did not cause any adverse events or safety issues in these patients [9]. As a limitation, we are not able to provide a consistent correlation between AIS and EEG-findings.
As a limitation, we are not able to provide a consistent correlation between AIS and EEG-findings.
Identifying AIS should lead to prophylaxis for stroke recurrence, like in any other AIS-patient. Since the duration of NCSE is associated with worse functional and cognitive outcomes [10], every effort should be performed to treat not only NCSE itself, but also to find and treat its cause.
In summary, AIS is a rare, likely underdetected but relevant etiology of NCSE. Hence, if the cause of NCSE remains unclear, a negative cerebral CT should be rapidly followed by brain MRI.
Notes
The authors have no financial conflicts of interest.